Embrace the Joke by Pat Conrad MD
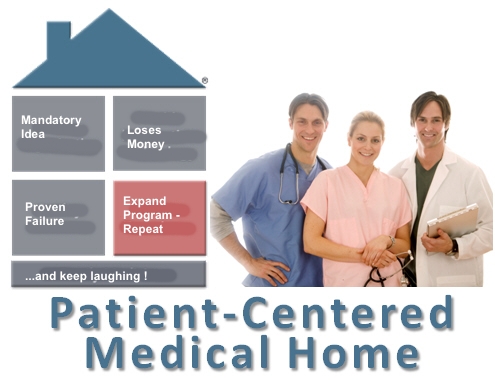
The amount of dishonesty that has now become the foundation and coin in medicine is maddening, disheartening, and funny. Watching goofy primary care types head fake themselves into worse economic shape has at least got to be good for a laugh. The good folks at Medical Economics will obviously print anyone (they’ve run my stuff a few times), and that includes Salvatore Volpe, MD, pediatrician, who cranked out a sweet primer on embracing the Primary Care Home concept.
Step 1: Accept the PCMH as good, necessary, and inevitable. The Patient-Centered Primary Care Collaborative “focused on quality and safety.” Hehehe, just try arguing with anything that favors quality, safety, puppies, or sunshine.
Step 2: Support your acceptance of PCMH by stating how big the problem is, inferring that magnitude defines imperativeness. “Population-based care is pro-active in nature and does not involve face-to-face interaction, is often uncompensated, and can account for more than 25% of the time” of the staff . So we gotta do something!!
Step 3: Justify the mandatory nature of the PCMH by rattling off a chain of acronyms that are the veritable ass abscesses of real practicing physicians: The Association of Academic Health Centers, The Joint Commission, the National Committee for Quality Assurance, and the Utilization Review Accreditation Commission, all organizations who preserve the safety of their own bank accounts by forever finding new faults with the “quality” of those doctors and hospitals who keep rolling belly-up for approval.
Step 4: Once an unsustainable idea is formalized, pack further layers of assurance around it. A high-sounding ideal must be defended, no matter how bad an idea it is in practice: “The Affordable Care Act led to varying degrees of enhanced reimbursement for Medicaid and Medicare providers while multiple commercial plans also offered to increase payment to practices that qualified. Unfortunately, these programs were not universally implemented and many are at risk of ending if not renewed by the federal and state governments.” But should not a practice that qualified be more efficient in controlling long-term costs? Should not such a practice be more cost-efficient in the short term, by the increased energy and timeliness of its clinicians as they are more able and motivated to jump on the email requests without having to see increased numbers in the lobby? Surely the bonuses for qualifying programs made up for any revenue shortfall from seeing fewer patients…?
Dr. Volpe shows that the PCMH concept is by his own definition unsustainable i.e. can’t work without subsidies from somewhere. He then – and this is the funny part – ignores this core fault and blames the failure of the concept on “these programs [not being] universally implemented.” Translation: this unworkable idea is not yet widespread enough: “The challenge for many practices is to provide PCMH care without adequate funding as we wait for value-based programs to become more prevalent.” And that is …
Step 5: Make a bad, mandatory idea too big to fail. “By joining accountable care organizations, PCMHs can leverage the infrastructure and finances of a larger group to help during the transition to a value-based payment system that benefits patients and providers alike.”
There is absolutely NO data that demonstrates that either patients or providers will be in any way benefitted by the PCMH model.
Step 6: See Step 1. Repeat as needed.









I love these comments sections!! They continue to show me that I am not only not alone, I am in agreement with the vast majority of people (physicians). Where the devil do these people in power come from? It ain’t the same place I come from! And they are so frequently wrong! And when it’s discovered that their ideas are wrong, do they say, “Oh, we were wrong. That didn’t work out. Let’s change it back to the way it was” ?? Nope, they actually double down…
Great analysis!
If you want to read one of the most hilariously dishonest articles ever published in a semi-reputable journal, go back and read this piece of shit from the Annals of Family Medicine that tells us how the PCMH is going to make us all rich:
http://www.annfammed.org/content/2/suppl_3/S1.abstract
It’s rare to see anything in print that is so consistently wrong on every single point – our thought leaders at their best!
That’s very funny, considering what the estimated costs are for maintaining a PCMH:
http://www.aafp.org/news/practice-professional-issues/20151021pcmhstudy.html
A British publication pointed out some issues perhaps fifty years ago with the concept:
We’ll be fighting in the streets with our children at our feet
And the morals that they worship will be gone
And the men who spurred us on sit in judgment of all wrong
They decide and the shotgun sings the song
I’ll tip my hat to the new constitution
Take a bow for the new revolution
Smile and grin at the change all around
Pick up my guitar and play, just like yesterday
Then I’ll get on my knees and pray
We don’t get fooled again
Just not sure of what the “morals” thing is all about, actually.
Also, I must object to your comparison to butt abscesses. Butt abscesses don’t INTEND to be a pain in the ass. Comparison to those ASSociations are insulting to perfectly natural pathology.
Or, as Morty used to say, back in the old neighborhood:
“I lose money on every piece…
… But I make it up in VOLUME.”