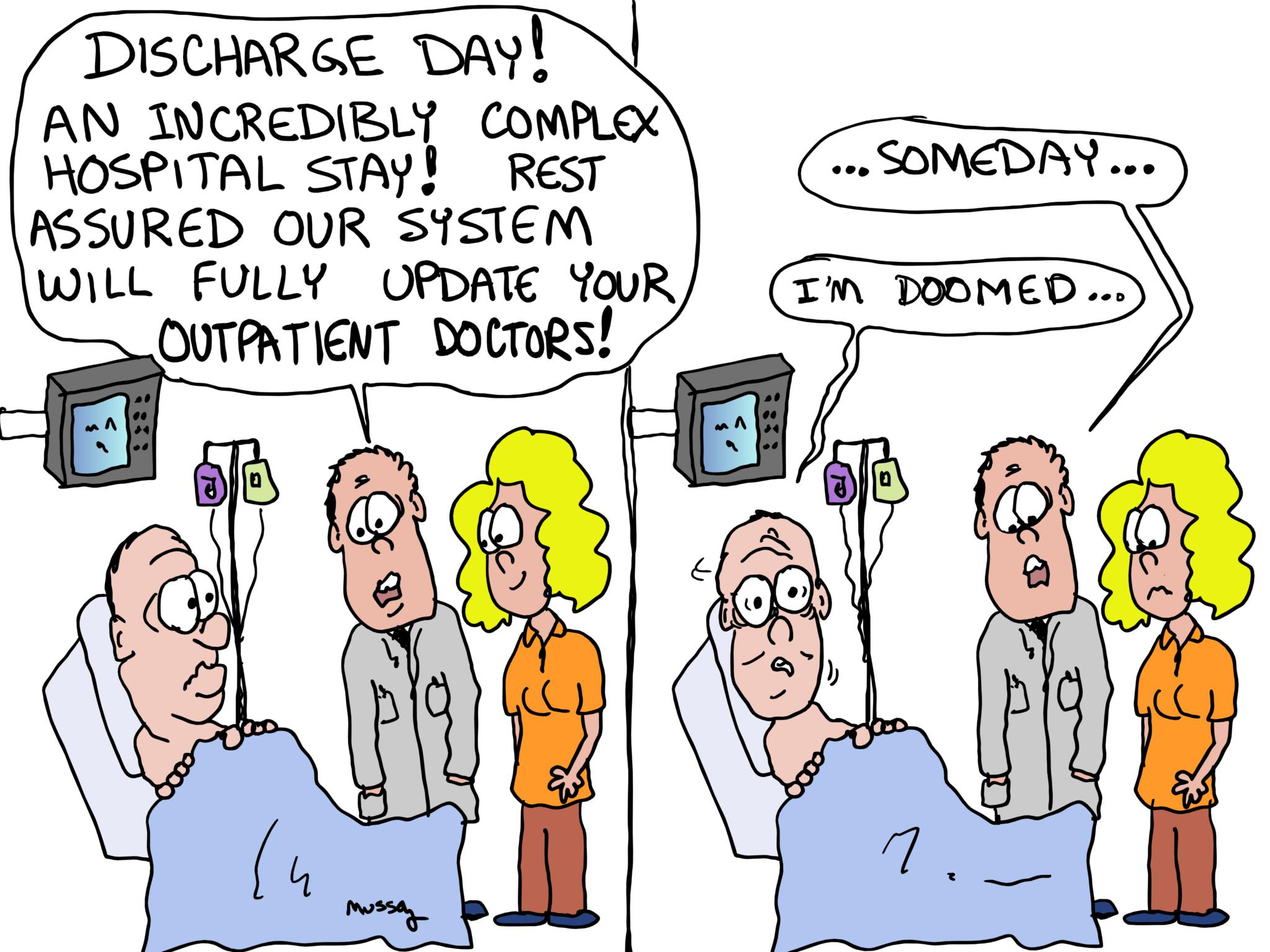
We Are Discharging You From The Hospital So Try Not To Die by Steven Mussey MD
We are discharging you from the hospital. Try not to die.
Please do yourself a favor and read this article from the Washington Post. The article is important, but it fails to capture the enormity of the problem.
Bottom line: When a patient transitions out of the hospital, the risk for preventable catastrophic medication errors goes through the roof. Yet, hospitals and physician offices are doing a terrible, awful, no-good job at communication.
The risk for failing to track serious issues becomes dangerously high:
“That lung nodule we found in the ER CT scan still hasn’t been worked up.”
“Your liver enzymes were really bad looking on discharge.”
Medications are radically changed in a hospital stay:
“Should I be on Xarelto AND Warfarin?”
“Should I stay on my Lisinopril with my Losartan and extra potassium?
Getting a discharge medication list into the hands of the receiving doctor or nurse is often impossible.
Getting a medical summary of any sort often takes a miracle. Getting a summary that has useful information is even more impossible.
Hospitals admit and discharge patients at supersonic speeds. Many tests are run and changes are made. Patients leave feeling bewildered.
A good hand off prevents death and injury.
Many hospitals spend all their time concentrating on arcane “metrics,” but consider communication with the receiving doctor to be a waste of time.
If your hospital is doing a good job, tell them.
If it is doing a bad job, scream loud and keep on screaming.
Your patient’s life depends on it.









This problem makes me miss the “social visit” I used to make to my patients who were admitted by a specialist. I made sure the patient understood what was happening and why. Making sure I knew what drugs had changed. Sometimes having my office call the patient in their room before they are discharge to schedule for their followup visit. Did I get paid for this….no. Tried may times but was denied for duplicate services, not enough documented in the note etc, etc.
So sad that the role of doctors was completely ignored in this article, and virtually all the comments. Blaming systems and the use of unqualified personel is important, but as long as no one thinks doctors should hand off care to doctors of lesser status, no one will. Why do I have to call the ER when sending a patient 911 with chest pain, when they are set up to deal with the general public doing the same thing? Why do I tell outpatient doctors I am referring patients to about the patient? It’s called professional courtesy and it improves care. But no one is courteous to me when I use my time to beg for information I need to do my job, and I usually give up, wondering why I was so naive as to try in the first place. Until primary care has enough prestige for someone to think I might need information to do my job and that my job matters, or even notices my absence in a story like this, these errors will remain ubiquitous.
Have you ever tried to contact the hospitalist to ask about a discharge? Have you ever RECOGNIZED THE NAME of a hospitalist who treated and discharged your patent?
The few times I tried to reach Dr. XBLFRT PNDWSQLKT at the hospital, I was offered nothing but confusion – that person was a locum, just on the migrant labor trail. I once tried to track down Dr. PNDWSQLKT, who was in Idaho, to ask about a particularly unusual patient – no recollection.
It’s not the hospitalists who are fragmenting the system – hospitalists ARE fragments of the system. We have handed over our healthcare to a superstitious belief that algorithmic medicine is more accurate than human medicine; and then built algorithms that cannot compete with an idiot child in their reasoning skills.
I received a call from a patient with nontrivial hematochezia. I told her to call 911 My reasoning was that the blood pipe had become connected with the ass pipe, and this should be located and fixed before all the blood came out. That is perhaps vulgar and primitive – but beyond the ken of our medical universe.
I was unable to locate an ER or an attending that she went to, for six hours. After that, I found the ER she had gone to. I practiced in the days where an OUTPATIENT ATTENDING could have a patient admitted to a hospital; no more. About thirty hours later, she was discharged with the assurance that her symptoms were just a mild viral illness – the incidental cold that she, in fact, did have that was not associated with the hematochezia. They dutifully gave her antibiotics and albuterol, and sent her home, where she was found dead the day after from a GI bleed.
We absolve the algorithm-makers and the management theorists from the attribution of evil to their actions; and blame things on Dr. PNDWSQLKT, who will have a performance ding on her/his locum transcript. Whatever.
It is social anosmia. We cannot smell fascism, even when it is ripe and bloated.
Two big reasons for this problem.
#1 EMR. It is great for compiling pages and pages of notes that are really just pre-fed in data input by a non medical person or old information that hasn’t been updated and that is very easily, with the click of a mouse, “imported” into a discharge note. Almost none of it relevant. Sometimes simply the volume of these notes dissuades a patient from even reading it due to it’s volume and complexity.
#2 The Hospitalist system. The patient’s primary care doctor rarely sees the patient in the hospital any longer. The doctor caring for the patient in house has to get to know a new patient every time and there is extremely poor communication between them and the primary when it is time for discharge.
Remember the days when the patient’s actual doctor took care of the patient both in and out of the hospital and when it was discharge time, he/she would simply TALK to the patient and tell them what to do/take after discharge and would hand write out all instructions on ONE sheet of easy to read and understand paper?
Yeah, we sure have made things better with all of our metrics and benchmarks haven’t we?
Our family doc finally quit doing hospital work when she was forced out by the hospitals requiring hospitalist only care. Didn’t matter though, there was no way she could keep up what with seeing patients in the office and then spending hours after patient care doing computer input so she could get paid. Marcus Welby is dead, long live Marcus Welby.
The late Dr. Welby died of his failure to recognize the medication error after his own hospitalization, and received 20mg of METHOTREXATE QD instead of METOLAZONE. Instead of diuresing his CHF overload, he diuresed his gut epithelium, then his bone marrow, and then his ticket to stay on this planet.
In the early nineties my hospital asked the physicians what was the biggest factor in length of stay. Here is what we came up with and the solution:
1) Foley catheters- Keep them out
2) Pre-existing co-morbidities-Make sure patient had good primary care follow-up
3) Family support-contact family to make sure they were involved
4) Need for step-down rehab- Create/expand step down facilities/home care
5) Home layout- Bed on ground level floor
Once these were done LOS decreased. However, over time for some reason these ideas were replaced with blanket LOS rules. Still don’t know why.