ABIM & ABFM Have Become Resistant Strains by Pat Conrad MD
The Twitterverse this week provided an interesting ripple when some physicians I follow expressed more than some mild outrage over the latest pro-MOC campaign from the ABIM. The ABIM – you know, the ones who make millions by extorting doctors via their Maintenance of Certification shakedown – are now intimating that the MOC saves lives: “New research indicates that physicians who participate in MOC, a lifelong learning and assessment program, screen women appropriately for breast cancer, potentially saving lives every year.” “Patients who saw internists certified after the MOC program was in place were 2.8 percent more likely to have annual breast cancer screenings and 1.7 percent more likely to have biennial screenings than similar internists not subject to the program requirements.” So either internal medicine residencies don’t TEACH breast cancer screening, or internists so addle-headed from sitting too close to their EHR screens can’t REMEMBER to screen women. Right? What other reasons, other than patient consent, physician judgment, or scare-tactic hype from Big Internists could account for this shocking disparity? This study eagerly trumpeted by the highly profitable ABIM was done by the Jacobs Institute of Women’s Health, whose funding I have not yet been able to learn.
“One of the most interesting findings was that several patients who had not been screened for breast cancer for a while did undergo a mammogram after the MOC program was in place,” said lead author Bradley M. Gray, Ph.D., ABIM Senior Health Services Researcher.”
The 12/17 issue of Family Practice News had an article suggesting that increasing the scope of practice for family physicians will reduce burnout. Amanda Weidner, MPH (who probably sees as many patients as the average hospital or insurance CEO) had some interesting findings. From all the would-be and current burnouts interviewed, she learned that those less likely to burn out practiced adult inpatient medicine, delivered babies, made house calls, and did procedures. Non-burnouts had “more areas of clinical practice.”
Weidner stated that her data indicated that the number of hours worked was not associated with burnout. The article did not mention how the study controlled for EHR’s, MACRA, MOC, ICD/CPT, increased patient wait times, declining reimbursements, medical malpractice suits, or similarly joyful primary care variables.
Here is a gem: “Maintaining a broad scope of practice for family physicians can help fulfill the ‘triple aims’ (enhancing patient experience, improving population health, and reducing costs) – now sometimes characterized as the ‘quadruple aims’ with the addition of preventing burnout – of health system performance, said Ms. Weidner.” If you don’t think this reeks, then that runny nose you’ve had isn’t snot, it’s cerebrospinal fluid. Why do I say so? “Ms. Weidner reported that her work was supported by an ABFM Foundation grant while she was a visiting ABFM scholar.”
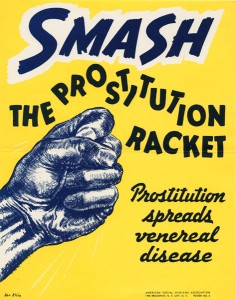
The ABIM is trying to scare women into demanding MOC as a way of continuing their funding stream. The ABFM is funding non-clinicians to tell clinicians that they should be doing more, to which the ABFM hopes to point as another demonstration of its own indispensability.









“Patients who saw internists certified after the MOC program was in place were 2.8 percent more likely to have annual breast cancer screenings”
USPTF doesn’t recommend annual screening for most women.
Does MOC make you a worse doctor?
Of course there is plenty of Bias in this non-randomized, controlled or blinded piece of junk science, being written by the ABIM exceutive staff including Lipner and Bradley M. Gray, Ph.D., ABIM Senior Health Services Researcher.
Not to mention that the whole breast and prostate screening routine has been flipping and flopping for a number of years now to save money-under the “choosing wisely” mantra of ABIM cost cutting paradigms.
who would believe this snake oil?
Just more gaslighting of US physicians:
http://drwes.blogspot.com/2018/01/moc-and-gaslighting-of-americas.html