Question: What do you get when you cross a mudslinger with a humdinger?

Answer: A Mundinger, the author who wrote – A Randomized Trial of Primary Care Outcomes in Patients Treated by Nurse Practitioners or Physicians (1). A mudslinger is a person who tries to damage someone’s reputation with accusations or insults. Mudslingers are always kept busy during political campaigns. If you spread rumors or gossip about another person, whether they are true or false, you are a mudslinger (2). A humdinger is defined as a striking or extraordinary person or thing That was one humdinger of a storm (3). A Mundinger (1) is the author of this article that I have written about before that keeps showing up in social media. In all seriousness, haven’t we seen enough of this 20-year-old research article (1)? I couldn’t resist the play on names. But isn’t it apropos to reference this article and the term mudslinger? Isn’t there this current push within some communities to denigrate physicians all the while promoting the (self-perceived) superiority of mid-level providers? In other words, mudslinging. The article(1) is full of untruth, bias, and data manipulation. The very first sentence: Studies have suggested that the quality of primary care delivered by nurse practitioners is equal to that of physicians. What studies? This sentence isn’t referenced. This lie has also been debunked with reviews of this purported evidence from other studies claiming the same, which was found to have poor methodology, poor quality, and just not true. This has become the rhetoric often touted as reasons to expand the scope of practice of nurse practitioners (NPs).
The referenced study “is a large randomized trial designed to compare patient outcomes for nurse practitioners and physicians functioning equally as primary care providers.” Here’s where I see another set of problems. Comparing apples to oranges, can you really do that? Can you compare apples doing apple work to oranges doing apple work? In other words, can you compare two different disciplines doing the work of one of the disciplines? Can you really ethically randomize a patient into groups where one of the groups has significantly less education towards doing the work of the other discipline? Also, the study references that the NP’s in the study were required to have collaborating physicians. As such, I think the purpose of this study is flawed.
Next, this study measured data from 1995 to 1997, in other words, 25-year-old data. How can this study still be relevant as such in 2020? The study then used data from 11 physicians and 7 NPs. I believe this is a significant limitation which affects the power of this study. The central hypothesis was:
“that the selected outcomes would not differ between the patients of nurse practitioners and physicians (1)”
However, if you recall, in the NP study group, each of the NPs was required to have a collaborating physician. Wouldn’t this set the standard of care to that of the collaborating physician and truly not measuring the difference between the physicians and the NPs? So of course the hypothesis would be true because they were measuring a physician group and a group of NP’s collaborating with physicians. I think this makes the hypothesis flawed. Another thought too, this kind of verbiage is often used to claim superiority.
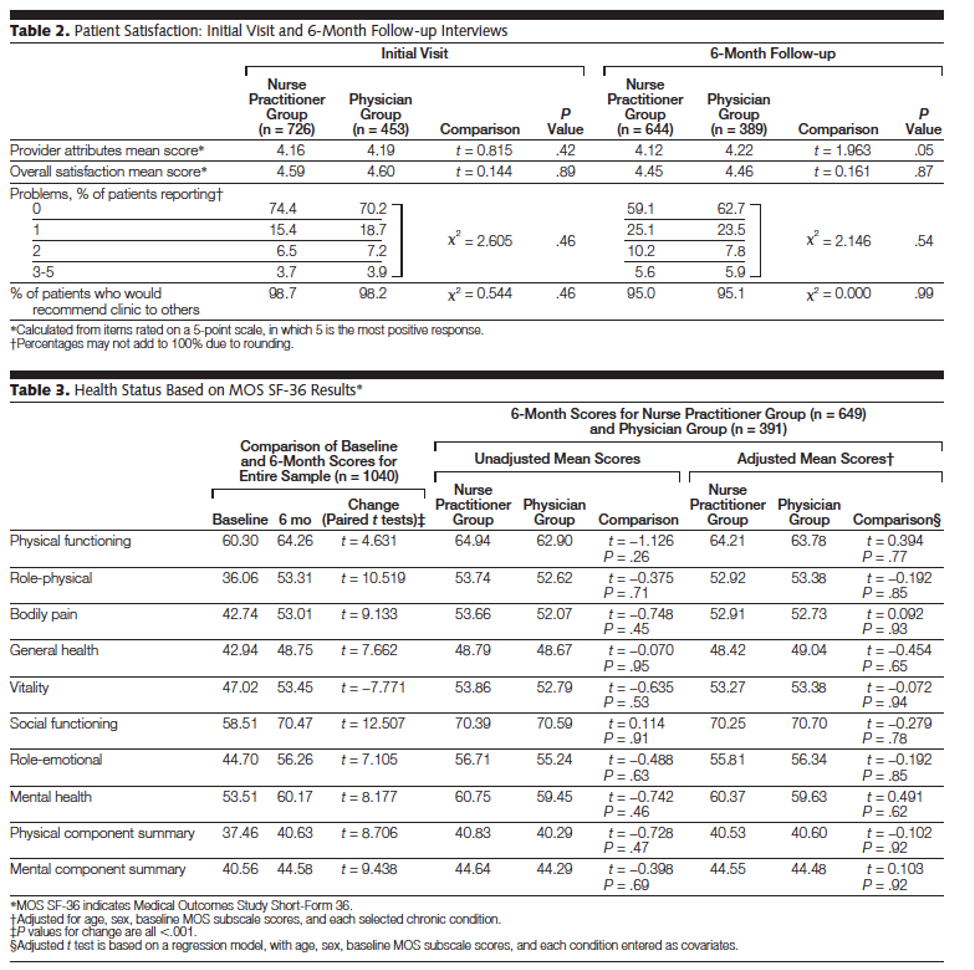
The study included patients with diagnoses of asthma, diabetes, and/or hypertension. Patients were followed up with at 6 months and 1 year. There were 1181 patients assigned to the NP group (7 NPs) and 800 patients to the physician group (11 physicians). Outcome measures were collected using the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36). According to RAND (4): As part of the Medical Outcomes Study (MOS), a multi-year, multi-site study to explain variations in patient outcomes, RAND developed the 36-Item Short Form Health Survey (SF-36). SF-36 is a set of generic, coherent, and easily administered quality-of-life measures. These measures rely upon patient self-reporting and are now widely utilized by managed care organizations and by Medicare for routine monitoring and assessment of care outcomes in adult patients. Seems legitimate but being a survey, I would suspect patient recall bias. I’m also not sure 6 months and 1 year is enough time to truly measure chronic disease indices.
Because I’m getting tired, I’ll skip to the results section. See the table below and make specific note of the P Values. I’m not sure what to make of that. I mean with those P Values as high as they are, it negates statistical significance. Or was that the point to be able to profess that no difference was noted between the groups? Is this data manipulation? I’ll leave it there.
References:
- https://jamanetwork.com/journals/jama/fullarticle/192259)
- https://www.vocabulary.com/dictionary/mudslinger
- https://www.merriam-webster.com/dictionary/humdinger
- https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html









I commented upon in another note. CMS has determined that NPs can perform both the administrative role and clinical work of the physiatrists.
CMS Releases FY 2021 IRF Proposed Rule
The Centers for Medicare and Medicaid Services (CMS) has released an ill-timed and shocking FY 2021 IRF proposed rule that includes a proposal to amend the IRF coverage requirements to allow non-physician practitioners (NPPs) to perform certain duties that are currently required to be performed by a rehabilitation physician.
CMS is requesting public comments on the proposal by June 15, including specifically whether commenters believe that quality of care in IRFs will be impacted by this proposal and any specific evidence that may help inform the issue.
Letter to the editor, Wall Street Journal yesterday. A cardiologist on a Washington political lobbying trip for that specialty. A group met their Congressional representative. The subject of electronic medical records came up. Congressman had the nerve to say that EHR’s May drive doctors to early retirement, but they will just be replaced with nurse practitioners.
According to the cardiologist, a NURSE PRACTITIONER in the group set the Congressman straight on that.
Now, there’s the obvious issue that if EHR’s drive physicians to early retirement, they will be equally frustrating to nurses, ultimately with the same effect. A point lost on the politician.
More to the point, maybe, is the reveal of what they actually think of you.
I can’t help but get angry when I hear the “hero doctors” line (and nurses, etc.) because you know for a fact they don’t mean it. They never meant it. Never will mean it. You do know for a fact, that when this blows over, the doctors, nurses, etc., will be thrown away like trash. The hospital administrators, insurance executives, and especially politicians. The instant the disease fear subsided, they will turn on you like a rabid dog.