The Metamorphosis of Medicine
Many of my articles for Authentic Medicine discuss issues around full practice authority(FPA) for nurse practitioners(NPs) and Optimal Team Practice(OTP) for physician assistants(PAs) which, in my opinion, are euphemisms describing the practice of medicine without a medical license. Certainly, their umbrella organizations have a vested interest in furthering these agendas as well. However, I would be remiss if I did not include the complicity of my own colleagues/profession in assisting, and even supporting, this insidious transition in medicine. I shared my perspective of this paradigm shift in an article I wrote over a year ago (https://authenticmedicine.com/2019/07/a-history-of-npps-a-personal-view/).
It has become apparent to me that some of my physician colleagues are either unaware of or don’t care about this troubling change in the quality, administration and unequal distribution of health care. Many have chosen to believe the hype, their complacency apparent with attitudes that “this is the future of medicine”, failing to recognize that in uttering that statement, they are willingly relinquishing their responsibilities as leaders in medicine to steer the course of health care. No longer the drivers in the discipline of medicine, they have relegated themselves to the passenger seat. They have surrendered–prepared to be marionettes controlled by the strings of the non-medical, non-scientific, corporate conglomerates and any other selfishly motivated entities running the business of healthcare.
There was a time when U.S. medicine was number one in the world…when physicians led medicine and patients had unimpeded access to their doctors. But two significant events occurred that shepherded doctors down the road to healthcare hell. The first: we sold our profession to corporations and private equity firms. We knew next to nothing about business at that time. Physicians were seeking long-term financial security and early retirement. Some believed these businesspeople would do right by them and their patients when they turned over their private practices. Because we docs are like that. We want to believe the best in people, even when they are stabbing us in the back and smiling in our face. Because we are by nature altruistic, we presume others are also. We assumed that their intent was genuine. We didn’t know these businesspeople were predators and we were the prey. They recognized the potential financial gains in the business of medicine and salivated, like Pavlov’s dog. And now we(and the patients) are paying the price. We have morphed into providers and the patients, commodities.
The second incident occurred when the Institute of Medicine(IOM), now known as the National Academy of Medicine(NAM), published a report in 2010 on the “Future of Nursing (https://pubmed.ncbi.nlm.nih.gov/24983041/)”, which then began the transformation of physician-led medicine to nursing-led. The IOM report was funded by the Robert Wood Johnson Foundation(RWJF), one of the largest charitable organizations in the nation and an active and fervent supporter of the “Future of Nursing: Campaign for Action”. The committee responsible for writing the report (https://www.ncbi.nlm.nih.gov/books/NBK209889/) had only two physicians on the panel, a pediatrician from Dartmouth whose research has included funding from RWJF, the Aetna Foundation and the United Health Foundation, and an internist who is the Executive Vice President and CMO of CVS Caremark. To insinuate that the committee was skewed would be an understatement.
“….Nurses therefore have valuable insights and unique abilities to contribute as partners with other health care professionals in improving the quality and safety of care as envisioned in the Affordable Care Act (ACA) enacted this year. Nurses should be fully engaged with other health professionals and assume leadership roles in redesigning care in the United States. To ensure its members are well-prepared, the profession should institute residency training for nurses, increase the percentage of nurses who attain a bachelor’s degree to 80 percent by 2020, and double the number who pursue doctorates. Furthermore, regulatory and institutional obstacles — including limits on nurses’ scope of practice — should be removed so that the health system can reap the full benefit of nurses’ training, skills, and knowledge in patient care. In this book, the Institute of Medicine makes recommendations for an action-oriented blueprint for the future of nursing.”
The problem was that there was no legitimate structured plan to guarantee that these “residencies”, “fellowships”, nurse practitioner and doctorate programs were standardized and measured up to the caliber required to accomplish the objectives envisioned by the committee. Nevertheless, it was imperative that this political agenda move forward by any means necessary. The numbers of nurse practitioners in the U.S. did indeed increase–by leaps and bounds. However, the quality of the nurse practitioners’ clinical competency did not demonstrate a concomitant mastery of advanced skills. This was predictable, particularly since some of the various nursing associations involved in the “Future of Nursing” campaign were aware of the unchecked proliferation of subpar online degree mills with questionable accreditation, the lack of clinical preparation and fundamental knowledge of graduates from those programs, increasing complaints of patient mismanagement and escalating malpractice payouts for NPs. It is what should have been expected when physicians were left out of the equation and plans to lead medicine were allowed to proceed with health care professionals trained in a nursing discipline that required no FORMAL didactic education or clinical training in the practice of medicine. Despite these issues, the politics of power, money and a clear, long-term purpose ensured that the timetable set forth by the report was not hindered by anything as trivial as inconsistent, non-standardized, poorly regulated NP programs throughout the nation. The IOM and the nursing organizations supporting the initiative forged ahead, undeterred.
Currently, limitations on scope of practice(SOP) for NPs, which were designed to protect the public, are indeed being removed throughout the country as FPA progresses. Since no real, consistent oversight exists in states with FPA, it is nearly impossible to monitor scope of practice and quality of care provided by nurse practitioners since regulatory measures were eliminated. Many state nursing boards are too overwhelmed and/or inadequate to effectively govern NP practice. Quality of care can only be assessed retro-actively, sanctioning the public to be the lab rats by which the yardstick gauging clinical expertise is measured–after the fact. In other words, the assessment of standard of care is based on patient outcomes–when it may be too late and the damage is done. This is not preventative care and is a deplorable and unconscionable act. Collection of data will only occur when, and if, a legislative, nursing or regulatory body sees fit to follow up standards of care and outcomes in the states with FPA. To date, none of these entities has deemed follow up necessary in any states with full practice authority. Not one. Apparently, presumption of excellence in the provision of care is a sufficient litmus test. It is important to note that with the exponential growth of nurse practitioners, physician assistants were slowly displaced from the medical landscape. In my opinion, PAs were forced to develop a strategy that would ensure job security. That strategy became what is known as Optimal Team Practice. Put simply, it was a matter of job survival.
An interesting irony is that in 2011, the IOM was instrumental in convening a panel of experts, the Panel on Understanding the Cross-National Health Differences Among High-Income Countries, to assess the reasons as to why the U.S. had significantly large health disparities compared to other high-income countries. The panel came up with a list of recommendations related to research and policy (https://www.ncbi.nlm.nih.gov/books/NBK154469/). Pursuit of national health objectives were also recommended and included the plan to “reform” health care. It is still not apparent to me exactly how the “Future of Nursing” fits into the solution to narrow the large health disparities, especially when most of the other high-income countries do not have NPs practicing as they do in the U.S. The higher quality of their health care systems is predicated on other contributing factors. The specifics of this planned reformation in the U.S. remains as vague as the scope of practice for nurse practitioners.
We physicians, and others who stand in opposition to this lunacy, have a chance to right this wrong. We have thousands of unmatched medical school graduates seeking any opportunity to strengthen their chances of getting into one of these limited residencies. I include IMGs and FMGs in these numbers because they are doctors also. Yet they are completely ignored by the medical establishment–treated like pariahs. If one chooses to believe the myth of the physician shortage, then why not utilize these doctors-in-waiting? Why aren’t we expending more energy finding options for them? Why are we more receptive to funding “residency” and “fellowship” programs for non-physician practitioners while unmatched doctors are left to fend for themselves? Assistant Physician(AP) programs(not to be confused with physician assistant), which enables these graduated medical students to work with docs in rural or community areas and maintain their skills until they can re-apply for residency, exist in at least 4-5 states. Why aren’t physicians sanctioning more of these programs? Contrary to popular belief, many of these students are excellent candidates, there simply were not enough residency slots available. Physicians could be supporting the federal bipartisan bill, the Resident Physician Shortage Reduction Act of 2019, which was introduced in the House in March 2019. The bill would increase residencies by 15, 000 over the next 5 years. So why aren’t t some physicians contacting their state legislators and pushing them to support this bill? Wouldn’t this be a better option if one is sincere about filling a physician gap? Well…much of this isn’t happening because physicians remain uninformed and unmotivated to act on behalf of these potential doctors. In addition, the intent of corporate bigwigs was never to increase the number of physicians–it was to replace physicians with cheaper alternatives who would ensure greater revenue. It was to replace physicians with more pliable options who would be less likely to resist the illegal interference of business in the provision of medical care. You see, the bylaws of every hospital clearly state that the ultimate decision of a patient’s care rests with the treating PHYSICIAN. Can’t dismiss that statement. Can’t bypass it. Can’t erase it. If the C-suite did, the hospital would own complete liability. The only way to address it was to remove the physicians…surreptitiously. Keep a few token, compliant docs for their licenses and get rid of the rest. Non-physician practitioners have no such protection under the bylaws; hence, they are less likely to resist corporate control and are therefore more desirable. To the detriment of physicians, the pandemic expedited this process.
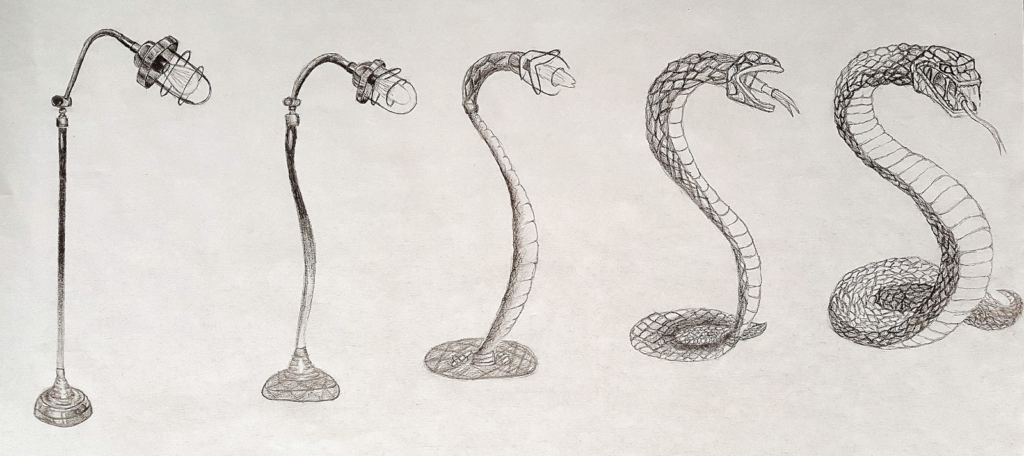
Physicians who resist this insidious and barely concealed attempt by corporate leadership to slither its way even further into the practice of medicine by proxy, under the guise of “collaborative team care”, are erroneously labeled as being anti-NP/PA–a commonly used trope designed to detract from the real conversation. Non-physician practitioners are as much cogs in this profit-driven machine as physicians and patients. The real intent, by corporations involved in the business of medicine, private equity groups, many of our so-called umbrella organizations and individual clinicians, is the complete transformation from the discipline and practice of authentic, humane, scientific, value-driven, patient-focused, physician-led medicine to a sinuous, investor pleasing, corporate-led, revenue-driven enterprise for slimy, greedy shareholders and their sycophantic facilitators, many of whom, unfortunately, are health care professionals.
Physicians, our eyes have been opened. It is time to take back medicine. It’s time.









Franz Kafkaesque…
I agree with your assessment. However, another issue is the attitude of upcoming students, residents, and fellows. Many do not want to go into the needed specialties as the “reward” is not sufficient. Much of our profession is only interested in working set hours and having several weeks’ vacation, along with other perks that accompany working as an “employee”. Only when the “screws are tightened” and restrictions, harassment, etc. occur that they see the light.
I have been in practice for over 37 years and have fought the corporate suits since 1982 when I started my residency. It has been worth it but it does drain one and is more difficult than appeasement and toeing the line. My battles have rewarded me with seeing my patients get what they needed and improving. However, it also had a CEO of a regional hospital accuse me of being disruptive for the audacity of disagreeing with him. Not many would want to go through that process.
Also, the comments by many within the large hospital systems are that NPs, PAs, and others are more financially efficient. This is an uphill battle. I am not sure that there are enough of us left to climb that hill.
Hello Dr. Newman, Unless your comments are published elsewhere, I only think a very small number of physicians are aware of the problem. I found out as I was a subscriber to the Placebo Journal and transitioned to Doug’s blog after that folded. I tell you as I came from a multi-specialty group, I’ve shared these concerns with some of my partners and mostly they’re too preoccupied with keeping their heads above water and are likely going to do what you’ve suggested. Retire as soon as possible. Another reason why docs in my state generally don’t care as so far, the NP’s have limited scope (but that could change) and have to work with a doc. Also if the doc works in a group or a “bussiness” they might been “encouraged” to collaborate with an NP whether they want to or not. I’ve seen docs forced to take an NP on when they didn’t want one.
I had an NP who worked with me for 20 years and previously was an oncology nurse before going back to school. She worked in the same pod as me and her exam rooms just around the corner in the open workspace. She retired before me as she was a few years older. Before all this FPA stuff became a concern she would tell me outright and unsolicited that FPA is idiotic. She recognized the broad scope of medical practice and wanted no part of working alone. She had ready access to me for case discussion and worked hard not to leave any loose ends. She always spoke highly of my intellect and I always came back I wasn’t the smartest in med school. I did pick up some extra pearls though as I was unmatched in 1982 did 2 years of a categorical surgery residency, transferred elsewhere ostensibly to go into Urology and was asked to do the 2nd year over again. I was single, unmarried and had my butt worked off. I was 195lbs of solid muscle when I started out. I worked so hard that after I left at the end of that year from hell I stepped on a scale and weighed 149lbs. My parents were shocked. I was terminated as I was baited into a non-medical argument with an attending about protocol, not a direct patient situation. I received a bad evaluation and the department head told me to get the guy to change it. I’d be d@mned to do that as he was wrong and I was right. Made one phone call at the prior institution where I came from and I got into an FP program. The next 2 and a half years were a piece o’ cake for me.
I too exited the field at age 63.5 July 1st because EHR, call and hospital practice was becoming too hard to keep up with. Mix in the stresses of MOC and having to go out of town to meet CME requirements as I was too tired at night to sit at a computer and diddle with it. A lot of primary care docs sit at home at night finishing up on EHR stuff anyways. Fatigue is a big factor too as I had to be Luproned for prostate cancer salvage. Had surgery, PSA didn’t go down as it was a peripheral lesion, choline PET showed a tiny bit in the bed where the prostate used to be, got radiation and Lupron for 2 years. PSA staying down at 4 years. Chemical castration leads to fatigue that I still deal with.
I was unmatched in 1982 and FP was my last choice but at least one can make a living and spaces were available back then.
I was unaware that there is a number of unmatched med students with no positions available now. Back in my day, states made “capitation” grants to med schools and residency programs to help defray the costs of education. Trying to ramp up new residency programs is going to be very tough without BIG money and oversight would be sorely needed to make sure they’re not turning out inferior physicians. The earlier that’s started though the better.
I can see now the big picture. Why have docs when a “cheaper” product (ie. FPA NP’s or PA’s) can be had? Why spend more money on residencies when one just needs to get more NP’s FPA? I now see where this is going. Too bad because as you have pointed out, patients are going to get hurt. I can foresee where FPA NP’s will be paying on the nose for malpractice insurance as they won’t have a collaborating physician to throw under the bus. Mark my words, the s#!t is going to hit the fan big time on this and unfortunately patients will die or be maimed due to this pathway to h&ll. Keep up the reporting please.
What can we actually do to help these medical students who do not match
1. Propose Assistant Physician bills like they have in Missouri, Arkansas, Kansas, Utah, etc.
2. Pester your legislator to keep pushing for passage of the Resident Physician Shortage Reduction Act.
It’s a start.
Dr.Newman;
Unless it starts to affect more physicians in their cash flow ,personally,you will not get much response.
By the time it does,it will be to late..Laws will be on the books and Nursing will be running the Show. Them and Administrators, Corporate CEO’s. MD’s/DO’s will be just another Employee. Easily replaced.. Fun Futures!! And you did it to yourselves.. All that knowledge, Arrogance, and
difficulty talking to people outside of Medicine. Competing to be the smartest in the room. So sad,such a letdown. Look at now,all the different opinions on shutdown/open up. Look at everyone pursuing their own narrow interests,hidden agendas. So much education. Everything is competition, Everything IS a Business model. Thank you