Supercalifragilisticexpialidocious: Paradoxicalanxioakatoniachromocytomaintoxicating withdrawal syndrome
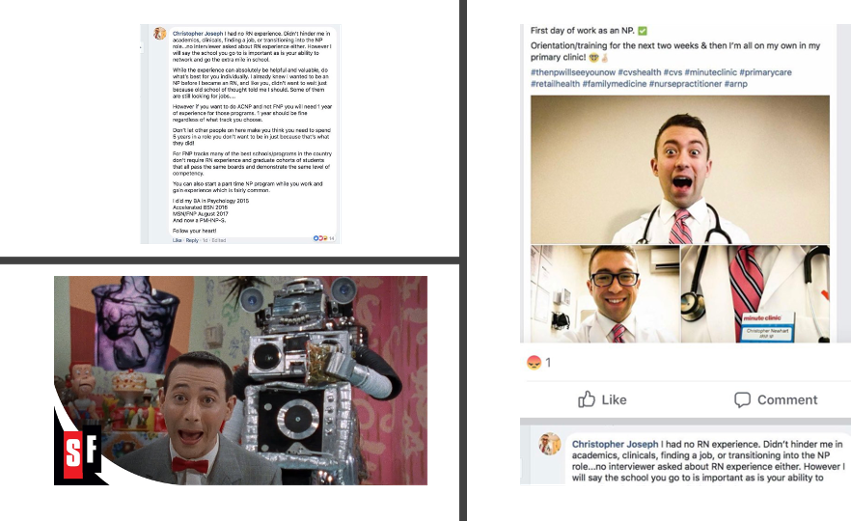
So, I’ve been seeing this picture making its way around social media. Then I’m seeing this tweet by President of the American Association of Nurse Practitioners (AANP) Sophia L. Thomas DNP, APRN, FNP-BC, PPCNP-BC, FNAP, FAANP (1). I couldn’t resist the play on Pee Wee Herman. Here’s my question Sophia, is this NP leading? I mean here you have a psychiatric nurse practitioner (NP) bragging about how he had no experience as a psych RN before taking a 2 year-course and now able to provide primary psychiatric services to a very vulnerable population. Here’s my suggestion as a former psych NP: clean your side of the street with this shoddy NP education model not requiring a minimum of 5 years clinical experience as an RN before becoming an NP. I was a psych RN for 15 years before I became a psych NP. Here’s what our little Pee Wee is going to miss not having psych RN experience:
Paradoxicalanxioakatoniachromocytomaintoxicating withdrawal syndrome
(Paradoxical-anxio-aka-tonia-chromocytoma-intoxicating-withdrawal-syndrome)
Patient presents with one simple symptom – severe psychomotor agitation. An experienced RN who just did the medication reconciliation notices the patient just started aripiprazole a week ago and quickly recognizes possible akathisia. The RN calls the covering NP, who just became licensed and had no prior RN experience, and together they figure out that a good course of action is to give propranolol and clonazepam. The patient then has a seizure, becomes more agitated, and vital signs are through the roof. The experienced RN then reviews labs with the new NP and notices the patient tested positive for cocaine and the experienced RN knows you shouldn’t have given a beta-blocker in a possible cocaine intoxication scenario. He/she isn’t sure why, but knows it’s not supposed to be done. The experienced RN also might know that sometimes patients given benzodiazepines have paradoxical excitation reactions. In an effort to control the seizures, knowing benzodiazepines can’t be used in this case, the new NP orders carbamazepine. The experienced RN is hesitant. He/she knows something about carbamazepine interacting with a lot of medications. 20 minutes later the patient now is diaphoretic, tremulous, more anxious, having stomach cramps, leg and back aches, and nausea, vomiting, and diarrhea. The experienced RN and new NP again review the labs and notice that the patient also tested positive for methadone and the experienced RN remembers doing the medication reconciliation with the patient on methadone. The experienced RN remembers knowing something about not giving carbamazepine to a person on methadone as it can precipitate opiate withdrawal. Too late. Since the patient’s vital signs and blood pressure are still elevated the new NP tries clonidine figuring it would help the blood pressure as well as the opiate withdrawal. The experienced RN doesn’t know why, but he/she is skeptical with a gut feeling, expresses reservation, but complies with the order. Nothing changes. Blood pressure still through the roof. Both are baffled. The experienced RN then suggests they call Dr. MD who is the supervising physician of the setting, but the new NP, full of Dunning–Kruger effect, professes they’ve got control of it. The experienced RN, while baffled, offers suggestions to the new NP and sees the patient is also a diagnosed schizophrenic with a history of catatonia, and has seen cases on the inpatient unit whereby rigid catatonic patients can sometimes become excited catatonic patients. The experienced RN knows that sometimes lorazepam is used in catatonia, but the patient just had a bad reaction to the clonazepam, so he/she suggests the patient may need Haldol to sedate to avoid injury. The new NP while having never heard of excited catatonia agrees to a trial of Haldol. 30 minutes later the patient is in the room, extremities tremulous, but neck turned to the right, rigid, and oral facial muscles frozen like. The experienced RN quickly recognizes acute dystonia and suggests Diphenhydramine. Having never seen acute dystonia, the new NPs confidence is starting to wax and wane, but they are too proud to call in the backup MD/DO. Still agitated with severely high blood pressure, the new NP, knowing the patient can’t tolerate Haldol, sees the option to use olanzapine IM injection and decides to re-challenge the benzodiazepine but with lorazepam IM. Before the experienced RN can intervene, a newer RN covering the experienced RN on a lunch break happily complies. The experienced RN returns from lunch and is furious as he/she finds their patient with excessive sedation and cardiorespiratory depression. He/she knows you don’t give both IM olanzapine and IM lorazepam together. Then without warning, the patient suddenly develops an arrythmia and dies. On autopsy, on top of it all, the patient had a rare pheochromocytoma.
So, is there any doubt now that our little Pee Wee’s of the world should have RN experience before becoming an NPs? I’ll leave it there. Perhaps this could be a starting point in the reconstruction of the ridiculously poor unregulated NP education diploma mills going on, that maybe Sophia could focus her efforts. I.e., clean up your side of the street, and we physicians will solve the physician shortage problem and lead heath care teams.
Word Table:
Paradoxical is the paradoxical excitation as a side effect of benzodiazepines.
Anxio equals anxiety.
Aka means akathesia which is an inner drive to move and unsettling restlessness.
Tonia equals catatonic excitation, a rare form of excited catatonia, and also represents acute dystonia.
Chromocytoma stands for pheochromocytoma.
Intoxication means stimulant/cocaine intoxication.
Withdrawal – self-explanatory.
References:
P.S. I’m applying to psychiatry residency match this year if anyone knows anyone or program directors, my application is in the ERAS system .









And after all this, somewhere there is a physician in the system, forced to take responsibility for all this.
Don’t care no more. A sizeable percentage of the American public can’t tell sh*t from Shinola, and will scream like babies when someone tells them too much truth. Close down the FDA, and let them buy what ever snake oil someone wants to market. You know billions are slushing around for the COVID vaccine – and likely any company in the vaccination industry could produce the equivalent. Meanwhile, we have fools who “party hearty” and get COVID. Have you heard anyone talk about HOW MUCH MONEY the treatment of COVID patients has cost us, has taken support and energy away from treating other illnesses? Nope! Covid gets treated by the tired-looking Magic Fairies in the gowns and gloves, and Somebody Else pays for a $100,000 hospitalization. Make America Great? I doubt the USA will survive another ten years on hospice. So go ahead – hand care off to people who burble garbage after their name. It doesn’t matter. Producing quality is a forgotten skill on the wind as the next Dark Ages come in. We may not be respected, but we can still tell when a patient ain’t gonna make it, and Uncle Sam’s gonna be in pine, presently. Who knew?
well written!