Short Changed: How to Address the Doctor Shortage

This referenced article made its way around social media recently. It is actually a response to a prior article Congress’s Doctor Shortage, Trillions for Covid relief, very little to address medical training (https://www.wsj.com/articles/congresss-doctor-shortage-11609802722?mod=article_inline). Those of us who follow this topic already know what they wrote:
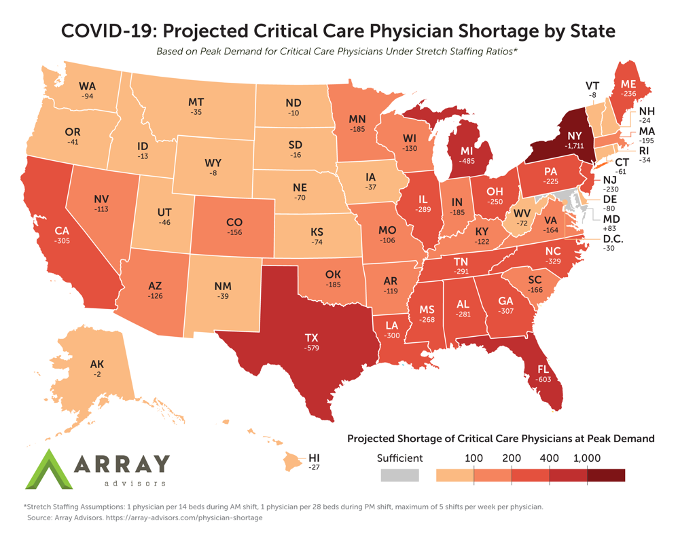
“Hospitals in much of America are triaging Covid-19 patients because they are short of staff, especially doctors trained in emergency-care and anesthesiology. Blame Congress, which rationed the supply of new physicians two decades ago and is only now addressing its mistake, albeit not nearly enough.”
This has been a contentious topic of discussion for many of us. Many of us profess that this is a physician problem to solve, and I believe it truly is, however it really lies at the hands of Congress. However, what I also mean is that it is not fodder for the advancement of scope of practice of mid-level providers. Unfortunately, this is precisely what has taken place. The physician shortage has become a weapon in the scope creep charade being perpetrated on the American lay public who don’t know any better. However, this article reports good news “The $900 billion relief bill adds 1,000 new Medicare-funded graduate medical education (GME) positions over five years.” Now some of you might say it’s a little too late, or not enough, and I agree with both of these sentiments, but at least it’s a baby step in the right direction.
Another problem Congress overlooked is the aging U.S. population and physician workforce. A third of the 906,000 or so practicing doctors in the U.S. are over age 60, and the Association of American Medical Colleges (AAMC) forecasts a physician shortage of 54,100 to 139,000 physicians by 2033. Shortages will be especially acute in geriatrics, primary and emergency care.
And then medical schools expand enrollment which increases graduation, but what happens is a bottleneck at the residency process. So, increasing med school positions does not increase the number of physicians as there isn’t a corresponding increase in residency positions. Then unfortunately, “Some health economists say technology and nurses can substitute for fewer doctors.” Nothing could be further from the truth. Only physicians can substitute for physicians. The responding article states “Physician substitutes including physicians assistants and nurse practitioners can often provide adequate but not equivalent care to board-certified physicians. If these substitutes were in fact equivalent, we should stop spending time and money educating physicians.”
The response article reports the problem as four-fold whereby (1) given the cost of the GME, “Restructuring graduate medical education by increasing the focus on community-based care and ambulatory-based surgery to supplement hospital-based care would result in a more cost-effective method for achieving this goal,” (2) “The second problem of health-care consolidation has been a result of obsolete antitrust laws that encourage health-care consolidation resulting in less competition,” (3) NP’s and PA’s are not physician substitutes, and (4) Approximately one-third of practicing physicians are over the age of 60 and more likely to retire.
There are some interesting comments to the article. Follow the link above.









The horse is indeed out of the barn. My father was hospitalized recently in my old hospital (I went outpatient only 5 years before retiring after 30 years attending there). He he did not see a physician other than a consulting pulmonologist the whole week he was in the hospital, just a couple of young NPs. NP #1 was supposed to be the ‘hospitalist.’ When I asked her what the “attending doctor’ thought about his prognosis she admitted to me that the doctor had never seen him “she just signs my charts.” NP#2 was from the palliative care ‘service’ who spent quite a while explaining why he was not hospice appropriate (fat lot she knew, he died within days of discharge). It became abundantly clear over the course of his hospitalization that the person with the most training and experience looking at this patient was ME. I don’t know if this is the norm in all the hospitals in my area but I intend to find out.
Now in this current EHR and such environment docs can’t wait to retire. I started residency in 1982 when there was talk there was going to be a physician oversupply. I didn’t match and stayed local in a categorical residency position. Transferred, got fired for speaking my mind about protocol that wasn’t a specific patient care issue and ended up in primary care/FP. I was very confident after 5.5 years of residency. I bet the University system where I went to school and residency is still wondering why I don’t donate money. Got sick of practice and left at age 64. Was rewarding when I started out but with more government involvement went downhill from there. It was a time of “classical” office, hospital practice and shared call was doable and satisfying. Forced EHR was a big part of destroying that. The early 2000’s started going to Hades. Now I believe most FP’s don’t do a mixed practice like the above and even fewer do OB. Just isn’t time to keep skills sharp having to do a pile of administrative paperwork.
Not surprising that primary care medicine is heading into the ‘ol W.C. (water closet). I wouldn’t tell graduating docs to go into it hence the “lelt’s” (A Doug abbreviation meaning Less Educated Less Trained) are moving in with disastrous outcomes.
Here in rural Central Florida, there are few independent physicians. Most all of them sold out to the hospital where they simply oversee rotating shifts of NP’s or PA’s. There is an increasing rumbling from the patients as they can no longer see their doctor (who sold out to the hospital) and at every visit there is a different “provider”. It is now so common when we ask who the primary care physician is, to get a response of “I only see Mary at Dr Smith’s office” (names changed to protect the innocent)……..I give up…..they are getting substandard care at the standard MD price!
“A third of the 906,000 or so practicing doctors in the U.S. are over age 60,”
From a simple Google search, “According to age statistics published by the Association of American Medical Colleges, the average age among medical students who matriculated at U.S. medical schools in the 2017-2018 school year was 24.”
That’s MATRICULATED. So graduation is age 28 on average (are there any three-year programs any more?). Residency AT LEAST three years, often longer. So the docs are in their early-mid 30’s when they enter practice.
Foreign medical graduates, I wonder if they are a couple years older on entry to USA practice, given time needed to gain immigrant status and possibly repeat of postgraduate training in home country and USA. I can’t say I have data on this, I would suspect foreign docs are at least the same age as USA docs or more likely older, on entry to practice.
Is it really surprising that a third of practicing doctors are over 60?
In youger days, I saw several docs who had to be pushed out because of illness. Passing out, angina attacks, they just could not do it any more. They were endangering themselves, let alone patients. Almost always, it was a heart-to-heart with docs more senior than I was at the time. Big retirement party at a banquet hall. Nurses came out of retirement to attend. Old pictures (….look, he had hair back then…..), old stories, presents, hugs and tears. And it was a shame, some of the docs I knew then, worked for free just to be around it, or seeing the patients no one else wanted. Saw the old docs in the doctor’s dining room (remember those?).
Now they take retirement like anyone else, and who can blame them.
That generation is gone. Good luck (with envy) to any doc who can escape this with some useful life left, to do something more productive and joyful.
Looks like everyone’s leaving New York.
That horse was out of the barn, the gate closed, and the horse gone over the hill, where he hitchhiked to town, then caught a train to the west coast, and got a job as a low-level coder in Seattle until forced to work at home by the lockdown.
For over 50 years, the citizens of this People’s State have come to see health care as an obligation of the government, thereby putting one of the most difficult pursuits into the hands of some of the least competent, most corrupt, and certainly dumbest creatures this side of the Black Plague, in the framework of a system philosophically designed to be incapable of dealing with such. We will all devolve to the level
of Med Techs, with special bonuses paid to the dwindling few who can perform a CABG (anyone can place a stent) or tease out an unruly meningioblastoma. One of the funniest things I ever hear is a patient bitching that they couldn’t get “their doctor” on the phone.
Speaking of the devil… I had a pre-op eval last week and on my data sheet, the “attending” was a NP. No mention of that. Just ATTENDING and her name. And this weekend on TikTok, a survey: who is more important, doctors or nurses.
Wow. It is spreading like wildfire.