A Brief Critical Read: Primary Care Provider Type – Are There Differences in Patients’ Intermediate Diabetes Outcomes?

“With growing evidence that the quality of care delivered by the professions is similar, this wide range in implementation of roles likely reflects organizational goals and cultures rather than the capacities of each profession. The results of this study suggest that physicians, PAs, and NPs can perform a variety of roles that can reflect the needs of the organization and patient population while maintaining quality of care. Although this adaptability can provide great benefit to healthcare delivery organizations and the system in general, conclusions regarding the “ideal” role should be approached with caution. More research on the effect of each role on access, cost, quality of care, and satisfaction of providers and patients is needed before answers will become clear.”1
A limitation up front is that I am biased toward Physician lead multi-disciplinary health care teams and this will undoubtedly influence my critique. This recent study1just emerged on the scene and social media. Let’s take a look. The above quote is the conclusion. Let’s dissect it. The terms “growing evidence”is cited in the reference section with references 28-32. However, it is beyond the scope of this brief review to analyze each article to see if they support the conclusion of equality among Nurse Practitioners (NPs), Physician Assistants (PAs) and Physicians (MD/DOs). I will pick one briefly2,3 (the first study listed below #28): (https://onlinelibrary.wiley.com/doi/pdf/10.1111/jan.13108) –
Publication biasis likely being published in the Journal of Advanced Nursing. Confirmation biasis possible whereby this type of bias is defined as: “Confirmation bias is the tendency to search for, interpret, favor, and recall information in a way that confirms one’s preexisting beliefs or hypotheses.”4 This study sample consisted of 271,003 patients identified as those having a diagnosis of DM2 and as being seen either by a primary care physician exclusively or an NP exclusively. From those patients, 199,185were seen exclusively by primary care physicians for 1,240,927 encounters (visits) and 4,385 were exclusively seen by NPs for 14,312 encounters (visits).3 Thus in a sample where MD/DO’s outnumber the NPs 46:1, this sets up a sampling bias:
(In statistics, sampling bias is a bias in which a sample is collected in such a way that some members of the intended population are less likely to be included than others. It results in a biased sample, a non-random sample[1] of a population (or non-human factors) in which all individuals, or instances, were not equally likely to have been selected. If this is not accounted for, results can beerroneously attributed to the phenomenon under study rather than to the method of sampling.)5
What’s interesting is this study didn’t actually measure the health outcomes of
Lower extremity amputation, HbA1c, Eye exams, Lipid screens, Flu shots, Foot ulcers but rather measured costs associated with these variables. And even these had interesting data. For example, the HbA1c outcome cost variable had a p value of 0.75. It is unclear exactly what this means from the study. Thus I would say that though this study is seen as evidence in the original article, the evidence is weak towards equating NP/PAs to MD/DOs in terms of quality of care and health determinant outcomes. Because it didn’t even measure the health outcomes, equality can’t be inferred.
Back to the original study, where the conclusion states: “this wide range in implementation of roles likely reflects organizational goals and cultures rather than the capacities of each profession,” – this statement negates the entire premise of equality among mid-level providers and MD/DOs. It infers that the capacities, capabilities, educational levels etc were not even explored or taken into account, but rather a function of roles within the organization. “These results suggest that physicians, PAs, and NPs can perform a variety of roles depending on the needs of the organization and patient population.”1 Notice it is not based on education, training, or skills of the provider types, but needs of the organization. The organization being the Veteran’s Affairs Health system. The article repeatedly mentioned team practice: “Based on theories of team effectiveness and roles, effective
incorporation of multiple providers into teams requires well-defined roles.” However, the roles of NP’s and PAs are not defined in terms of scope of practice as it relates to level of education and training, it rather defines primary care provider, and lumps PAs and NPs into this role. Thus redefining what is typically known as primary care physician to primary care provider and changing the operational definition. I’m not sure what kind of bias this is, perhaps confirmation biaswhereby it is the belief of the authors that this is the definition rather than the true definition, thereby negating objectivity.
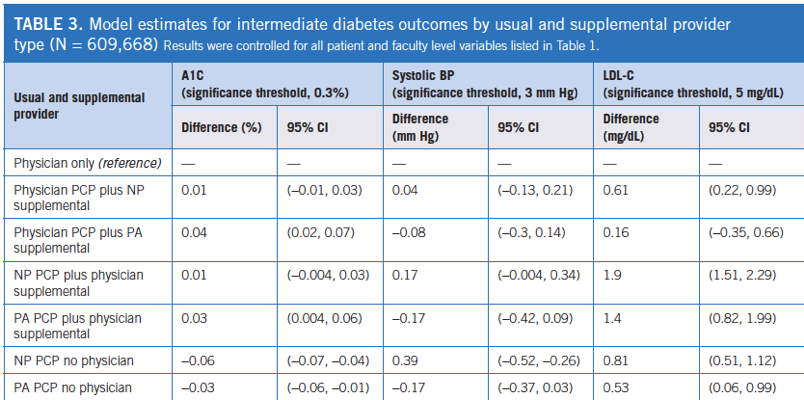
This study also had sample bias: “Physicians were the usual providers of care for about 77% of the patients and PAs or NPs were the usual providers of care for about 22% of the patients. About 14% of patients received all of their primary care from PAs or NPs.” As such, it does not seem possible for results or data to be analyzed with any veracity. In addition, the sample was obtained from interventions already accomplished as part of the individual’s standard care (a snapshot in time)– this was not the case where patients were randomized into provider groups as in a true randomized control trial(RCT). Thus, to establish equality as being professed, you would need the rigor of the RCT. The data table rather than the categories of providers being listed as independent variables, the physician only category became in essence the gold standard measure or dependent variable by which other category of providers was measured. It would seem that before and after values per provider category would better capture the data as it is unclear what the values of the physician only category was prior to the start of the study. Was there a larger or smaller delta to truly be able to compare provider categories? What were participants initial values and then the values after a period of time – but that would be a RCT and this was not. The premise here is that you can take a cross sectional set of individuals and stratify them into provider categories and the results either support or refute the hypothesis of equality among provider categories. However, this is not possible. If anything, the results of this study could be used as starting points from which to now base a RCT off of. The results are simply a snap shot of outcome variable data and not the results of interventions purposely being used to measure a delta. Thus with the statistical approach, the true change in health determinants was not accounted for. Thus negating the study from concluding equality or quality of care among provider types. Thus the study didn’t measure what it set out to measure: equality and quality of health care among provider types. To do this, you’d need a set of untreated diabetic patients, measure the initial set of outcome variable data, randomize them to provider groups, and in 1 year, re-measure the outcome variables and compare the delta, then compare provider groups. .
Ok, next topic……….
“this study adds additional support to the conclusions of previous studies that patient outcomes are similar for those with physicians, NPs, and PA as PCPs,”
I would counter that it does not. It simply measures snap shot variables, looked at who the providers were, and conclude equality. There was an inherent belief that mid-level providers are adaptable and can function on par with physicians.
“Although this adaptability can provide great benefit to healthcare delivery organizations and the system in general, conclusions regarding the “ideal” role should be approached with caution.More research on the effect of each role on access, cost, quality of care, and satisfaction of providers and patients is needed before answers will become clear.”
Overall, this study made an attempt to study and measure something hotly debated in 2019, however it fails to do so. Are there differences in patients’ intermediate diabetes outcomes? For example the A1C, what were the before and after values among provider types such that the delta could be captured and perhaps this could be statistically analyzed to truly do a comparison. As in the data table, measuring all changes among provider types against physician only values implies the physician only category is gold standard like. Thus, differences in intermediate diabetes outcomes by provider type are not adequately captured.
Have a great day.
REFERENCES:
- Everett, CM. (2019). Primary care provider type: Are there differences in patients’ intermediate diabetes outcomes? Journal of the American Academy of PAs: June 2019 – Volume 32 – Issue 6 – p 36–42. doi: 10.1097/01.JAA.0000558239.06875.0b. https://journals.lww.com/jaapa/fulltext/2019/06000/Primary_care_provider_type__Are_there_differences.8.aspx#pdf-link
- https://www.ncbi.nlm.nih.gov/pubmed/31136399
- Lutfiyya MN, Tomai L, Frogner B, et al. Does primary care diabetes management provided to Medicare patients differ between primary care physicians and nurse practitioners? J Adv Nurs. 2017;73(1):240-252. https://onlinelibrary.wiley.com/doi/pdf/10.1111/jan.13108
- https://en.wikipedia.org/wiki/Confirmation_bias
- https://en.wikipedia.org/wiki/Sampling_bias
- https://www.news-medical.net/news/20190610/Study-backs-use-of-physician-assistants-nurse-practitioners-for-treating-VA-patients-with-diabetes.aspx?showform=printpdf









How many readers read the article under discussion and believed the conclusions – thinking that such voluminous studies must support the conclusions drawn by the article writer? This sort of “soft lie” or “truthy” reporting has become routine in our sound-bite oriented media. No wonder we have the extremely low quality field of politicians up for selection on voting day!