A Take on Evidence Based Medicine: A Biased Report
“A systematic review that combines biased pieces of evidence may unfortunately give another seal of authority to that biased evidence.”(1)
And there it is…… From a bona-fide expert on meta-analysis and systemic reviews. Thus from this perspective, negates the findings in Impact of the Advanced Practice Provider in Adult Critical Care: A Systematic Review and Meta-Analysis based on bias.(2) (https://journals.lww.com/ccmjournal/Abstract/2019/05000/Impact_of_the_Advanced_Practice_Provider_in_Adult.13.aspx).
A hot topic these days. However, how many times have we heard the perfunctory “evidence shows,” or “from the evidence,” or challenges to “show me the evidence?” Well,“’evidence-based medicine’ has become a very common term that is misused and abused by eminence-based experts and conflicted stakeholders who want to support their views and their products, without caring much about the integrity, transparency, and unbiasedness of science.”(1)
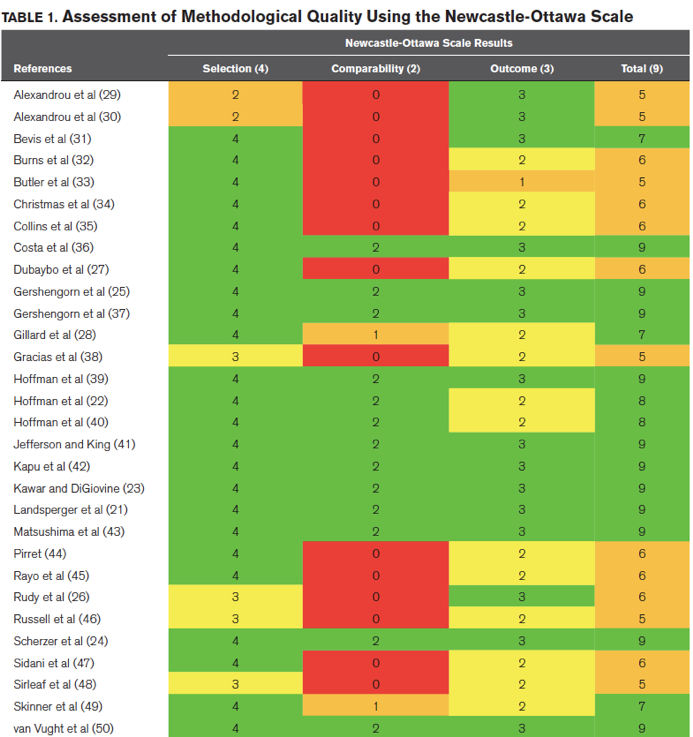
The systemic review referenced here states “for more than 2 decades, acute care nurse practitioners (ACNPs) and physician assistants (PAs) are increasingly embedded in ICUs, particularly in the United States. Which is true, but this meta-anlysis is based out of The Netherlands which could limit the generalizability. Only two of the lead researchers reviewed and chose studies for inclusion in the meta-analysis. The same two authors used The Newcastle-Ottawa scale (NOS) was used to assess the methodological quality of the included nonrandomized studies. This 9-point scale is based on three domains: 1) selection of the cohort, 2) comparability of the groups, and 3) quality of the outcomes. High-quality studies have a score of greater than or equal to 7, whereas moderate- and low-quality studies have scores of 4–6 and less than or equal to 4. “The NOS is a tool commonly used in medicine for the assessment of quality. Although it is a validated instrument and with a long history of reliability it suffers from several limitations. Other tools (tailored for cross-sectional studies and with more univocal items for other observational studies) are probably needed.”(4). That being said, it renders the included studies suspect for bias and poor quality confirming the notion of the aforementioned process of combining biased studies to form a biased conclusion. Moreover many of the included studies were rated by the researches as poor in the domain of cohort comparability.
“This review and meta-analysis shows no differences between acute care given by advanced practice providers compared with physician resident/fellows measured as length of stay or mortality.”
On the surface this sounds good. However, the leap being made is that both groups provided equal care because the outcomes were the same. The outcomes ……….. (a) mortality and (b) length of stay: I would counter that these outcomes don’t necessarily equate to equal care. These don’t really seem to me to be ethical nor free from financial constraints measures. Mortality – if you died it was poor care. Maybe it was great care but due to disease process there was mortality. We all know length of stays get cut short by insurance constraints. There’s no way to tell. In addition, it doesn’t account for mid-level and resident attending physician supervision thus in essence negating the ability to draw a difference in the groups as it is equaled out by the attending physician on the team. The equalizer.
Lastly, from the review itself:
“The results of this meta-analysis have to be interpretedwith caution. Although this review gives an overall view on the effects of APPs in the critical care setting, with a selection of the evidence-based cohort studies gradable by NOS score, there are differences in design of the studies which are also reflected by the sometimes high heterogeneity in the meta-analysis. In addition, the conversion from medians to means necessary for the comparison may introduce bias by itself as LOS usually shows a skewed distribution. Furthermore, regarding the NOS scale, no structural evaluation of bias was performed.”
REFERENCES:
- https://retractionwatch.com/2016/03/16/evidence-based-medicine-has-been-hijacked-a-confession-from-john-ioannidis/
- https://journals.lww.com/ccmjournal/Abstract/2019/05000/Impact_of_the_Advanced_Practice_Provider_in_Adult.13.aspx
- Ioannidis, J.P. (2016). Evidence-based medicine has been hijacked: a report to David Sackett. Journal of clinical epidemiology, 73, 82-6 . https://www.sciencedirect.com/science/article/pii/S0895435616001475
- https://www.wjgnet.com/2308-3840/full/v5/i4/80.htm








