Update in Primary Care: Depression in Primary Care May Actually be a Vitamin D Deficiency
BACKGROUND
Major depressive disorder (MDD) is a significant worldwide health problem, and often seen in primary care with comorbid medical problems such as hypertension, chronic pain, cardiovascular disease, diabetes, asthma, and others. There is a high instance of patients seen in primary care to where depression is either contributing to the physical health ailments, sequela of physical health problems, or a primary disorder in and of itself. Patients will often seek care in primary care settings versus purely behavioral health settings. Often in certain locations, the only healthcare option is primary care. It is therefore wise for primary care practitioners to be mindful that a significant portion of their patient population may in fact be suffering from depression. There are many identified factors, causes, and theories on the etiology of depression, and several different mechanisms are involved in the pathophysiology. One such mechanism that has been associated with depression is vitamin D deficiency. Vitamin D is a unique neurosteroid hormone that may have an important role in the development of depression. Some studies have demonstrated a strong relationship between vitamin D and depression. In a nonscientific convenient sample of the authors last 10 patients diagnosed with MDD on an inpatient psychiatric unit, 6 out of 10 (60%) screened positive for either vitamin D deficiency or insufficiency. It is unclear whether vitamin D deficiency was a contributing cause of the MDD, sequela resulting from the MDD, or associated with factors relating to the psychiatric patient population in general. However, given the evidence of (a) the association between vitamin D and MDD, and (b) the prevalence of depression seen in primary care; routine vitamin D screening and supplementation would be advantageous.
DISCUSSION
MDD is among the most incapacitating conditions in the world and is the single most frequent psychiatric disorder in the USA, with an estimated lifetime prevalence of 16.6%(1). Depression is often comorbid with chronic medical diseases (angina, arthritis, asthma and diabetes), and can worsen associated health outcomes and therefore will in fact be seen in primary care (2). Comorbid depression was identified in 9% to 23% of individuals with one or more chronic physical diseases emphasizing the importance of providing safe and effective treatment to people with co-morbid dual diagnoses (2). The National Association of State Mental Health Program Directors (3) reports that “10% of all Health Centers patients (primary care) have a primary or secondary diagnosis of drug or alcohol dependence, or severe mental health disorder (anecdotally this number is much higher, up to 50%).” Evidence suggests, for example, that between 10% to 40% of individuals seeking primary care have diagnosable mental health problems (1&4). Primary care emphasizes continuity, comprehensiveness, and coordination to meet the needs of persons with both chronic illnessesand chronic mental illnesses, such as depression. Patients often engage with health care by first presenting to the primary care provider (5-6). The top five health conditions (mood disorders, diabetes, heart disease, hypertension, and asthma) account for 49% of total healthcare costs and 42% of illness-related lost wages. Of these, mood disorders (depression is a mood disorder) rank third in healthcare costs, first in work loss costs, and second in total costs (7-8).
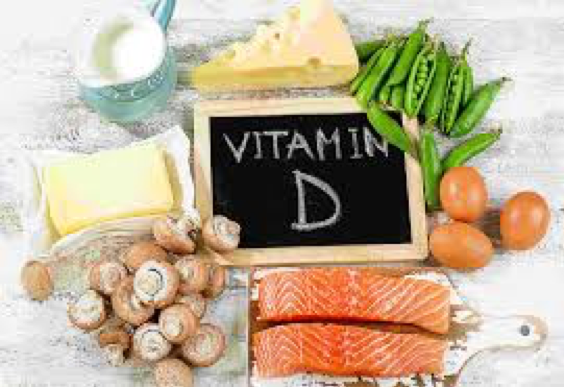
Studies have demonstrated a strong relationship between vitamin D and depression (9-10). Vitamin D is considered a neurosteroid hormone with receptors present on neurons and glia in many areas of the brain including the cingulate cortex and hippocampus, which have been implicated in the pathophysiology of depression (11). Vitamin D is involved in numerous brain processes and brain development,making it biologically plausible that it is associated with depression. It is therefore sensible that vitamin D supplementation might play an important part in the treatment of depression in primary care (12-13).
CONCLUSION
Depression is associated with significant disability, mortality and healthcare costs. It is the third leading cause of disability in high-income countries,and affects approximately 840 million people worldwide (13-15).Over two-thirds of the populations of the USA and Canada have suboptimal levels of vitamin D (13, 16-17). Both depression and vitamin D deficiency will be seen in primary care. Vitamin D, is a neurosteroid hormone associated with depression, and with numerous skeletal and non-skeletal functions with receptors and enzymes required for metabolism throughout the brain (18). Because of (a) the high prevalence of vitamin D deficiency, (b) the high prevalence of depression, (c) the association between vitamin D deficiency and depression, and (d) the prevalence of patients with co-morbid conditions presenting in primary care; there are public health implications. Public health implications include (a) cost, (b) providing care to patients with depression that might not otherwise receive care, (c) identify individuals deficient in Vitamin D that otherwise might not receive care, and (d) obtain better outcomes by simultaneously treating both chronic medial and mental health problems. Therefore, effective and comprehensive health promotion in primary care would potentially include both vitamin D screening and vitamin D supplementation. This is both coast effective and low risk. Primary care providers should consider Vitamin D screening and supplementation as part of their routine practice.
REFERENCES
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602.
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858.
- National Association of State Mental Health Program Directors (NASMHPD) (2005). Integrating Behavioral Health and Primary Care Services: Opportunities and Challenges for State Mental Health Authorities. Final Technical Report, January 2005.
- Agency for Healthcare Research and Quality (AHRQ). Integration of Mental Health/Substance Abuse and Primary Care. Evidence Report/Technology Assessment Number 173.AHRQ Publication No. 09-E003. 2008;October. US Department of Health and Human Services.
- Simon GE, Ludman EJ, Tutty S, et al. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial.[see comment] JAMA 2004 Aug 25; 292(8):935-42.
- Adler DA, Bungay KM, Wilson IB, et al. The impact of a pharmacist intervention on 6-month outcomes in depressed primary care patients General Hospital Psychiatry 2004 May-Jun; 26(3):199-209.
- Ford, D. M.D.,M.P.H., Decision Support/Depression. Power Point presentation to HRSA Health Disparities Collaboratives National Congress, September 2004. Based upon materials from Cole et al and Egener et al.
- Bartels, S. M.D., M.S, Integrating Mental Health In Primary Care: An Overview of the Research Literature PowerPoint presentation to NASMHPD Technical Report: Behavioral Health/Primary Care Integration— Guidance for Public Sector Implementation Work Group, June 2004.
- Wilkins CH, Sheline YI, Roe CM, Birge SJ, Morris JC. Vitamin D deficiency is associated with low mood and worse cognitive performance in older adults. Am J Geriatr Psychiatry 2006; 14: 1032–40.
- May HT, Bair TL, Lappe DL, Anderson JL, Horne BD, Carlquist JF, et al. Association of vitamin D levels with incident depression among a general cardiovascular population. Am Heart J 2010; 159: 1037–43.
- Eyles DW, Smith S, Kinobe R, Hewison M, McGrath JJ. Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroanat 2005; 29: 21–30.
- Fernandes de Abreu DA, Eyles D, Feron F. Vitamin D, a neuro- immunomodulator: implications for neurodegenerative and autoimmune diseases. Psychoneuroendocrinology 2009; 34 (suppl 1): S265–77.
- Anglin, R.E.S., Samaan, Z., Walter, S.D., McDonald, S.D. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. The British Journal of Psychiatry (2013) 202, 100–107. doi: 10.1192/bjp.bp.111.106666
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006; 367: 1747–57.
- The World Health Organization. Mental Health Gap Action Programme: Scaling Up Care for Mental, Neurological, and Substance Use Disorders. WHO, 2008.
- Ginde AA, Liu MC, Camargo CA. Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Arch Intern Med 2009; 169: 626–32.
- Langlois K, Greene-Finestone L, Little J, Hidiroglou N, Whiting S. Vitamin D Status of Canadians as Measured in the 2007 to 2009 Canadian Health Measures Survey. Health Reports 82-003-XPE: 8. Statistics Canada, 2010.
- Holick, M.F. Vitamin D Deficiency. NewEngland Journal of Medicine 2007; 357:266-281July 19, 2007DOI: 10.1056/NEJMra070553
(Editor’s Note: I believe we are dealing with a sun deficiency which leads to a Vitamin D deficiency. The studies adding back D pills are mediocre, at best. The studies with sunshines are better. Just my 2 cents. – Farrago)
Get our awesome newsletter by signing up here. We don’t give your email out and we don’t spam you.








