The Match and The Resident Physician Shortage Reduction Act of 2021
THE MATCH. The tortuous, yet exciting day when soon-to-be graduating students will discover where they will be attending residency. This long tradition is a double-edged sword of anticipation, however. Some grads cry out of happiness. Others from despair, because they did not match. They now have to go through the depressing Supplemental Offer and Acceptance(SOAP) process and hope they find a position. Back in my day, we called it “The Scramble” or scrambling because that is literally what we did. We clamored for any open positions in the specialty we were seeking. Usually, we were informed about those openings through our schools who were contacted by programs desperately seeking to fill their slots. Most of us were lucky and ended up in a program somewhere. Today, that is not the case. Nearly 10, 000 medical school graduates per year go unmatched because of a residency bottleneck. The result of an overproduction of medical schools without a concomitant increase in residencies, thanks to the residency cap enacted by Congress in 1997. This cap was placed to avoid a glut of physicians being produced; therefore driving demand down and thus, compensation. Unfortunately, there was no consideration of the fact that as medicine progressed, people would continue to live longer and require more care and more physicians. No thought that physicians would age and decrease their hours or retire and need replacements. There was no re-assessment of the situation until it was too late. And there was no way to shorten the medical education process without compromising quality of care. Ultimately, the expected glut became a “gap”. In a desperate attempt to address this impending shortage of physicians, more medical schools opened. As one would expect, when trying to address an imminent crisis haphazardly and without strategic planning, the “solution” failed to recognize that there would be no residencies for a large number of these graduates to enter. Hence, too many potential doctors with nowhere to train and no way to pay their outstanding, substantial debts. Those who benefited the most from this astounding lack of forethought were the medical schools profiting from these students.
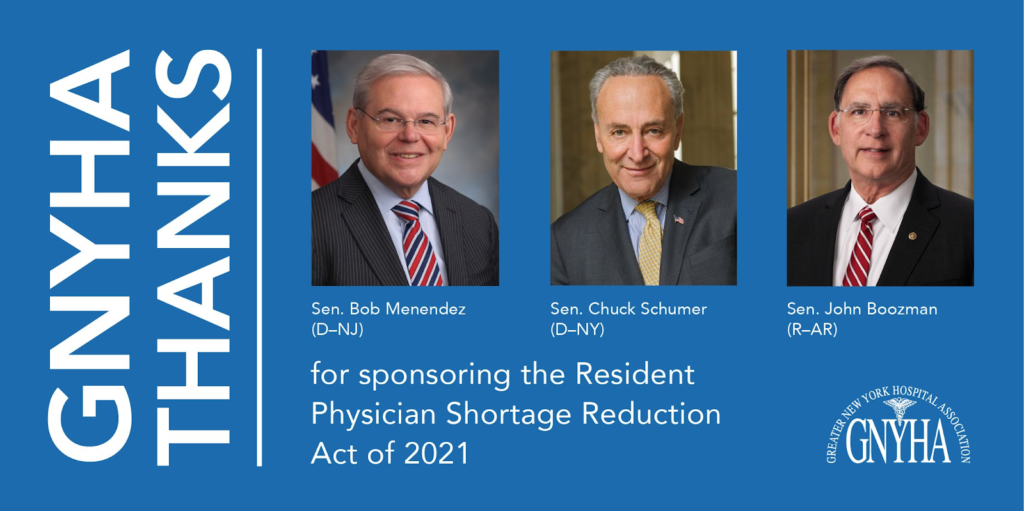
A bipartisan bill, the Resident Physician Shortage Reduction Act, was introduced in March 2013 by Representatives Joseph Crowley(D-NY) and Michael Grimm(R-NY) to address the looming physician shortage. It was shelved. Approximately every 2 years it has been reintroduced. And shelved again. In December 2020 it failed. Died. Was laid to rest in peace. Eight years after the original bill, it has been resurrected from the dead. Reintroduced once again as the Resident Physician Shortage Reduction Act of 2021. It would open 2000 residencies per year for 7 years. Thanks to the sponsoring senators who understand that this country needs more physicians and won’t give up trying to get this bill passed. Imagine if the bill had passed in 2013….Where would be today? Perhaps the residency bottleneck would not be as severe and we would have more docs who matched. We will never know because the bill was squashed. Over and over and over again. Instead, the focus seguéd to prioritizing the business of medicine by saving money and increasing the profit margin by replacing physicians with non-physician practitioners(NPPs) who were touted as being “basically” equivalent to physicians. Miraculously, GME funding somehow materialized to finance “residencies” and “fellowships” for these non-physician practitioners, purportedly to better prepare them to practice “medicine” in an effort to fill the physician gap(which in actuality was a cover for profit-making schemes). The “physician gap” became a selling point to convince legislators that the farce of NPPs filling a mythical space supposedly created by a lack of physicians was an altruistic move in the best interest of the public. And the ploy worked. Then COVID happened.
We all witnessed the immediate overwhelming demand for critical care docs, emergency physicians and hospitalists. Those administrators and physicians making these desperate requests actually used the term “physician” and not “provider”, which indicated to me what I already knew–the term “provider” was meant to conflate. But there was no conflating when it came to this pandemic. It became apparent there was no interchangeability between physicians and non-physician practitioners. Suddenly our roles as physicians were well-defined and respected. Begrudgingly. Because the powers that be were forced to acknowledge that we physicians are indeed irreplaceable.
What some may have not noticed is now that the pandemic is “chronic” so to speak, the demand for primary care physicians has skyrocketed. Patients are hesitant to go to hospitals for fear of getting COVID. Many people are unemployed and/or have lost their insurance and simply cannot afford the emergency department. Going to a clinic is cheaper and perceived as safer. The same primary care physicians who are usually dismissed and disrespected by colleagues and assumed to be easy to replace by NPPs are rising to the challenge. As usual. The PC docs have always been there…invisible. Doing their jobs diligently and quietly in the background, managing patients with multiple co-morbidities so efficiently that it appears they don’t do much. They make it look easy to practice primary care. So much so that many assume anyone with a modicum of medical training can do what PC docs do. All the while they get paid s**t. But now we see their value. Because they now have the added burden of managing post-COVID patients with all their still emerging post-COVID sequelae and pre-existent disorders/diseases. I was pleasantly surprised while perusing the web to find that their compensation is increasing. It’s about time. Hospital-owned and private clinics are getting overwhelmed with patients. PC docs, if nothing else, are efficient as hell. Clinic administrators recognize that it is not wise to ignore the potential dangers that may be percolating in post-COVID patients in the aftermath of their illness. Those subtleties require the expertise that PCs possess and have polished over years of training and/or practice.
I remain unconvinced that residents are not applying to primary care residencies. They are. It appears that a significant number of unmatched grads applied for positions in Internal Medicine and Family Medicine. Many U.S., IMG and FMG graduates have a great desire to practice primary care, despite the stigma about pay and respect.
If we are serious about addressing the lack of available primary care physicians practicing in this country, then we need to stop talking about filling the gap with non-physician practitioners. Every single health care professional in this country should support the Resident Physician Shortage Reduction Act of 2021. Contact your congresspeople and ask them to sponsor the bill and help push it through. It is about time we support these industrious future doctors who earned the right and the opportunity to become physicians.
Unmatched doctors….WE SEE YOU.
I would like to extend a heartfelt thank you to the Greater New York Hospital Association(GNYHA), in particular, Jon Cooper, Senior Vice-President–Government Affairs, for putting this issue of the residency cap front and center.









I don’t think there was ever a physician glut or any prospect of one. What were those people smoking?
What the author should propose is not an expansion of all residency spots but simply an expansion of primary care spots.
I disagree with this article. The majority of the 10,000 people that mentioned are people who went to Caribbean medical schools. They had questionable undergraduate records resulting in not matching in the US MD or DO medical school and the education and many of these places is also questionable both in basic science and then in subsequent clinical rotations. Deciding you want to live the dream, and going to a offshore medical school does not guarantee you the right to be a medical doctor. The number of residency spots is now fairly approximate to the number of medical school graduates in US MD and DO medical schools. Others are foreign medical grads which are badly needed in their home countries. Residency spots that were given to these people existed for two reasons. Originally they were supposed to obtain training and return home to their own countries. This rarely happens. Man y of these foreign medical grads are from well-to-do families and their home countries rather than disadvantaged and their own countries have a severe shortage. When countries like Ghana have one surgeon for every 200,000 people but yet we let their graduates come here to practice cosmetic surgery I don’t think we are fulfilling that need. The other reason these residency spots used to exist is the New York hospitals were so badly funded in such a bad experience that only foreign medical grads would fill these positions.
In addition many others who don’t match are insistent on trying for high-paying specialties rather than primary care despite not being competitive for those positions. Then they don’t match.
1. FMGs come from many countries, including the Caribbean. Of foreign med schools, a majority of U.S. citizens attend those in the Caribbean. And they typically do the last two years of clinical rotations in the U.S.
2. No one can simply attend any medical school in the world then apply for residency in the U.S. It doesn’t work that way. For a FMG to enter residency in the U.S., they have to attend a medical school that meets the standards and curriculum of U.S. medical schools(as determined by the LCME) and is approved by the U.S. Department of Education(USDE). If a school does not meet that standard, that graduate has to begin again if they want to practice in the U.S. That means from pre-med courses on. For a foreign school to receive such accreditation, it takes on average 10 years. For students to be able to take the USMLE and apply for residency, their school has to be listed in the Worldwide Directory of Medical Schools(WDOMS). So no, any foreign medical school graduate cannot stroll in off the street and become a medical resident in the U.S. They have to meet strict criteria.
3. Individual graduates decide where they want to practice, regardless of their citizenship. It is not yours nor anyone else’s place to tell them where that will be or should be.
4. Plenty of physicians who wished to practice primary care applied and did not match during this cycle. The NRMP needs a major overhaul because something stinks to high heaven.
5. The grads who do not select wisely in the match pay the price. Hopefully, they will learn from their mistakes and choose better when they apply in the next cycle.
6. What we do not need is NPs/PAs, under the guise of a “physician gap”, filling slots meant for actual physicians. We can use not only U.S. grads to fill the gap, we can use IMGs and FMGs. They are all physicians.
7. Pressure your representative to support the Resident Physicians Shortage Reduction Act of 2021. It will open up more residency slots, mostly in primary care.