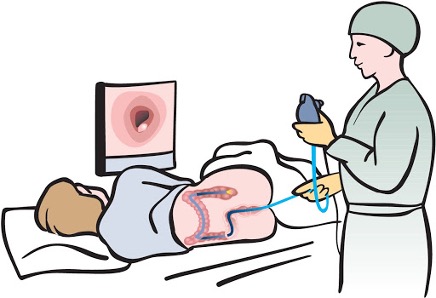
Colonoscopy Sh%t Show, A Different Kind of Scope Creep (Experience of nurse practitioners performing colonoscopy after endoscopic training in more than 1,000 patients)
I’m not bashing mid-level providers here, but in my opinion, the notion of nurse practitioners doing colonoscopies, and this study amounts to a Colonoscopy Sh%t Show! More scope creep, literally! The article referenced here is:
Riegert M, Nandwani M, Thul B, Chiu AC, Mathews SC, Khashab MA, Kalloo AN. Experience of nurse practitioners performing colonoscopy after endoscopic training in more than 1,000 patients. Endosc Int Open. 2020 Oct;8(10):E1423-E1428. doi: 10.1055/a-1221-4546. Epub 2020 Sep 22. PMID: 33015346; PMCID: PMC7508647.
In full disclosure, I am not a GI specialist, nor did I work in GI as a former NP. I was in psych. The closest I came to a colonoscopy was actually having one, and working in my surgery clerkship in med school with an outstanding general surgeon. Butt, who am I? I mean even The American College of Gastroenterology (https://gi.org/advanced-practice-providers/) has mid-level provider resources. The argument becomes that you can train the skill. Butt, going just by education alone, Gastroenterologists go through med school (4 yrs.), Internal medicine residency (3 yrs.), GI fellowship (3 yrs.). Compare that to perhaps the best trained NP with a bachelor’s of science in nursing (4 yrs.), master’s of science in nursing nurse practitioner (2-3 yrs.) then either on the job training or a NP GI fellowship (https://www.hopkinsmedicine.org/gastroenterology_hepatology/education_training/nurse_practitioner_fellowship_program.html) (1 yr). So, you can see the difference. But the notion of years of training and hours of clinical supervision and training is almost a moot point faulty argument, because there is a bigger missing point: physicians are trained in the medical model and nurses are trained in the nursing model. Thus, making this almost a non-argument. When the NPs that read this feel compelled to attack me, hold on for a minute. Wait……. What we have here is the same dichotomy that exists between BSN prepared RNs and licensed practical nurses (LPNs). The professional versus the technical. The more educated in critical thinking and theory versus educated in skill sets. The same ones who will be inclined to attack me, will be the same ones that profess angst against the LPN being equivalent to BSN/RN’s. And rightfully so. They are not. They might be able to do some of the same skills and tasks, but does that make them equals? No, they are different. I wrote about scope creep previously, and I think NPs doing colonoscopies is in the scope creep realm: https://authenticmedicine.com/2020/11/hey-creep-patients-deserve-care-led-by-physicians/. One might argue about the skill requirements to essentially stick a tube up someone’s rear end, butt it’s so much more than that. I digress, you know how I feel about NP’s doing colonoscopies, now back to the article.
While I readily admit my bias on this topic, the first thing I try to look at is bias within the article. I was only able to ascertain the credentials of the lead/corresponding author as a doctor of nursing practice (DNP), nurse practitioner (NP) – listed as CRNP –certified registered nurse practitioner and not colorectal NP. Since the article aim is “to assess the quality of colonoscopy performed by three gastrointestinal fellowship-trained nurse practitioners (NPs),” there is a high risk of author bias. Author bias defined as “opinion or prejudice that affects that author’s writing and prevents the author from being completely neutral about the topic or issue about which s/he is writing.” If an NP that does colonoscopies wants to see evidence “demonstrating that adequately trained NPs can perform colonoscopy safely and effectively,” (the actual study conclusion), this conclusion would likely be a foregone conclusion setting the study stage for bias along the way.
To give credit where credit is due, there is a lack of data on the topic of study in the literature. Thus, the notion to add to the body of knowledge is respected. Overall, the literature which they cite is non-conclusive and not sufficient enough to support the study conclusion. Makes you wonder how you can obtain IRB/Ethical approval for procedures which aren’t delineated in your scope of practice nor supported in the literature?
Current literature on the performance of non-physicians in endoscopy is limited, ………. much less is known about the performance of non-physicians in colonoscopy. This lack of evidence prompted a 2009 statement by the American Society for Gastrointestinal Endoscopy (ASGE) that “there is insufficient data to support the use of non-physician endoscopists to perform colonoscopy”
Literature is limited as they suggest. This is true. One of the studies they referenced was:
Day LW, Siao D, Inadomi JM, Somsouk M. Non-physician performance of lower and upper endoscopy: a systematic review and meta-analysis. Endoscopy. 2014;46(5):401-410. doi:10.1055/s-0034-1365310
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4153714/)
Upon digging in this study, one finds the following:
- a sensitivity analysis was performed examining the effect of procedure indication (screening versus diagnostic), provider type (nurse versus midlevel provider), and study design (observational versus randomized controlled trial) on outcome measures for flexible sigmoidoscopy. Such a sensitivity analysis was not performed for studies involving colonoscopy given that there were too few studies available (N=3).
- Among studies that involved colonoscopy there was insufficient data to perform meta-analyses comparing non-physicians to physicians with regards to polyp detection rate, adenoma detection rate, colorectal cancer detection rate or adverse event rate; however there was no difference between non-physicians and physicians in cecal intubation rates
- there were few studies available in which meta-analyses could be performed with respect to specific endoscopic procedures, particularly with colonoscopy and upper endoscopy, thereby limiting the generalizability of our results.
- This lack of data has resulted in the American Society of Gastrointestinal Endoscopy concluding there was insufficient data to support non-physician endoscopists performing colonoscopy and upper endoscopy: American Society for Gastrointestinal Endoscopy, Ikenberry SO, Anderson MA, Banerjee S, Baron TH, Dominitz JA, Gan SI, Harrison ME, Jagannath S, Levy M, Lichtenstein D, Shen B, Fanelli RD, Stewart L, Khan K. Endoscopy by nonphysicians. Gastrointest Endosc. 2009 Apr;69(4):767-70. doi: 10.1016/j.gie.2008.11.006. PMID: 19327469.
From this 2nd study where they refence too little literature pertaining to nurses and colonoscopies, when looking deeper, 2 of the studies were of nurses and in the Netherlands, and only one study was in the United States with mid-level providers: Limoges-Gonzalez M, Mann NS, Al-Juburi A, Tseng D, Inadomi J, Rossaro L. Comparisons of screening colonoscopy performed by a nurse practitioner and gastroenterologists: a single-center randomized controlled trial. Gastroenterol Nurs. 2011;34(3):210–216 (https://pubmed.ncbi.nlm.nih.gov/21637086/). “The goal of this study was to compare accuracy, safety, and patient satisfaction in screening colonoscopy performed by board certified gastroenterologists (GI-MD) and a gastroenterology trained nurse practitioner (GI-NP).” I guess to study a topic, you have to start somewhere, butt what is interesting, is that it is labeled as a RCT with 2 groups. One group to the GI trained NP with an N=50, and one group with 2 GI-MDs with an N=100. Can you really generalize findings with only 3 providers (1 in the GI-NP and 2 in the GI-MD) and with the GI-MD group having 200% more participants? I’m not knocking this study, but just pointing out a couple items that might refute the conclusion: “Using well-trained NPs for screening colonoscopy can be an effective strategy to increase access to colorectal screening.”
Ok, lost yet? Back to the original article:
Riegert M, Nandwani M, Thul B, Chiu AC, Mathews SC, Khashab MA, Kalloo AN. Experience of nurse practitioners performing colonoscopy after endoscopic training in more than 1,000 patients. Endosc Int Open. 2020 Oct;8(10):E1423-E1428. doi: 10.1055/a-1221-4546. Epub 2020 Sep 22. PMID: 33015346; PMCID: PMC7508647. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7508647/pdf/10-1055-a-1221-4546.pdf
First the premise: “the current workforce of gastroenterologists is unable to meet the needs for colorectal cancer (CRC) screening.” Says who? Where is this referenced? I believe this is nothing more than a strawman argument supporting the scope creep of NPs doing colonoscopies.
Second, the aim of this study “was to assess the quality of colonoscopy performed by three gastrointestinal fellowship-trained nurse practitioners (NPs).” I don’t think an N of three is generalizable.
Third, the method: “This was a retrospective study performed at a single tertiary academic medical center. Colonoscopies performed by three gastrointestinal-specialized NPs after having completed training of at least 140 supervised colonoscopies were reviewed for analysis.” How did this even receive IRB/ethics approval? It did state “Institutional review board (IRB) approval was obtained prior to initiating data collection.” But it doesn’t state what entity.
Fourth, the sample: “The study included 1,012 subjects (mean age 56.2 years, female 51.5 %, African American 73.9 %) who underwent screening colonoscopies by three NPs.” Is it me or does it seem that there is something ethical about the majority of the study population being AA?
Fifth, the conclusion: “demonstrating that adequately trained NPs can perform colonoscopy safely and effectively. With the demand for colonoscopy exceeding the supply, non-physicians could be part of the solution to meet the demands for CRC screening.” The conclusion is hardly generalizable with limited to 3 NPs. And again, the new talking point is becoming there’s an exceeding colonoscopy demand that must be met. And that only NPs can fill this made-up gap.
Now, to be kind, maybe properly trained, the task can be completed. However, having been to NP school, there isn’t the level of detail in training anatomy, physiology, pathophysiology, gross and micro anatomy, nor pathology when compared to medical school. I can only imagine how intensified this is with actual residency and fellowship. To the same extent, an LPN again could be trained to complete the task of orthostatic vital signs, but the BSN prepared registered nurse is educated and trained to interpret the normal versus abnormal findings and when and when not to notify the physician.