There Is No Substitute For Time Well Spent by Vance Lassey, MD
A while back I read an article on KevinMD entitled “How to make the most out of rushed physician visits.” I surmised that this article was going to be a mess, and I was right.
I am not trashing on the author, Dr. Dhand. He is simply a victim like so many other doctors stuck inside our broken system, and trying to work with what he’s got. And like the others, I’d say he suffers from learned helplessness. The bottom line is that most doctors just continue to practice some form of medicine that down deep they recognize could be done much better, rationalizing it with the mantra “That’s just the way it is.” They fail to see a way to do it right, or fail to take whatever courageous steps they have recognized could be taken to make things better.
The author’s learned helplessness is demonstrated here:
“…physicians are not afforded that luxury…this time restraint issue only seems likely to get worse. The question then is not how do we keep wishing for that utopian amount of time, but rather, how do we make the most out of the time we have and use it to its maximum potential?”
Dr. Dhand and countless doctors just like him do have more time to spend with their patients, they’re just being made to waste it, clicking boxes, filling out forms for insurance companies, attending useless meetings and so on. And they call a situation devoid of those intrusions, where they would have ample time for patients, a “utopia” (i.e. impossible).
Dr. Dhand kindly offers 2 solutions to the problem:
Solution 1: Make better use of nonverbal communication, because nonverbally, one is theoretically able to do upwards of 90% of the necessary communication.
I take it that what he’s getting at, is that if a doctor is constantly looking at her watch, staring at a computer screen, and has her hand on the doorknob, etc., the patient will be unsettled, and it will negatively affect the entire interaction. You THINK? This is common sense. Whatever deleterious effects poor nonverbal cues are responsible for, those effects pale in comparison to the effects of insufficient time spent. An 8-minute appointment with somebody who does not appear to be in a hurry isn’t much better than an 8-minute appointment with somebody who does.
And with regard to the idea of improving nonverbal communication: can’t we agree that it takes more than body language and 8 minutes to establish rapport, educate, counsel, console, empathize, and truly care for someone? While I will agree that friendly body language is very important in the realm of patient-doctor communication, simply demonstrating a relaxed demeanor is grossly insufficient to fix the problem of having only a fraction of the time we need with our patients.
Solution 2: “…[allocate] a certain amount of uninterrupted talk time for the patient (while actively listening)…use…open-ended questions, and [allow] time for a summary at the end of the consultation.” He also goes so far as to assert that …“None of these involve adding more time or putting a huge amount of effort in…”
In America, a patient is given a whopping 11 seconds to state their problem, before their physician interrupts them. That is insane. It’s inexcusable.
Sadly, interrupting his patient is the reality of any doctor who’s trying to get in his quota of patients, click enough EMR boxes to not get yelled at by some administrator, try to be less than 2 hours behind, fill out paperwork ad nauseum, and try to eat, sleep, and actually see his family.
So Dr. Dhand is right: asking patients open-ended questions and actively listening to their response IS the best way to practice medicine. But it’s certainly not going to “[turn] 10 minutes into 20,” as he claims. The opposite is much more likely: it might turn 20 into 40… and rightly so.
And we know beyond a doubt that spending more time to summarize the visit with the patient will contribute to better compliance, and probably better outcomes, higher satisfaction, all of it. But shorter visits? By saying stuff twice? Who can do something twice in less time than it takes to do it once? Do the laws of time and space not apply to Dr. Dhand’s exam rooms?
If Dr. Dhand had renamed his article “Providing better care by spending more time with patients,” then he’d have the beginnings of a great article. Instead, he describes a way to increase the quality of the patient visit, but one that would indeed exacerbate the not-enough-time problem.
So the true solution to not-enough-time-to-spend-with-patients is…find a way to free up time to spend with patients. Everything else is secondary. Learned helplessness has blinded too many doctors to the ways we can do this, but it boils down to this: Doctors must couragously fight the system that holds our time hostage.
My solution was Direct Primary Care.
Outside of the nightmare that is third party payers, nobody tells me how many patients I have to see in a day or how to do my job. I click boxes for no middleman. My low overhead allows me to offer mostly 1 hour visits, housecalls, and an expanded scope of practice, all while keeping my prices far below the prices inside the system. The result is that I can do all the communication Dr. Dhand refers to, exactly the way he recommends. I have a relaxed nonverbal communication style that tells my new diabetic patient we’re not rushed and she is free to tell me whatever she wants. I actively listen rather than stare at a screen the whole time. I can ask open-ended questions and she has all the time she needs to answer them. Then, at the conclusion of our visit, we can recap all of my education and recommendations, and she can teach that back to me. I know she’s got it. Now, she can go home, make some changes to her diet, and her diabetes is suddenly under control without meds. Health care, not sick care and chart care. Inside the system, I’d have been encouraged to interrupt her, give her 7 minutes, throw an expensive script at her and spend the next 10 minutes clicking boxes, before going to the next patient to provide more shabby care. Indeed, I’d have been rewarded and incentivized to practice that way.
DPC works for me, allows me to better care for the poor in my area, and much more. But there are other ways to fight back without leaving the system.
Maybe you are looking for ways to spend more time with your patients, but hesitate to really crush the reset button like my DPC colleagues and I have. Great news: you have no duty to suffer, and you can stand up to abuse. Tell the insurance companies you’re not their clerk, and you’re not going to fill out those forms unless they pay you to. Tell your administrator to take their patient quota and shove it. You’re the doctor–you’re generating the money that pays their salary, and last time I checked, the person writing the checks is the boss. Tell them to stop wasting money and wasting your time. Skip the next worthless meeting and instead spend an hour with a patient truly in need. It’s past time for medicine to be taken back by the ones who are in it for the right reasons.
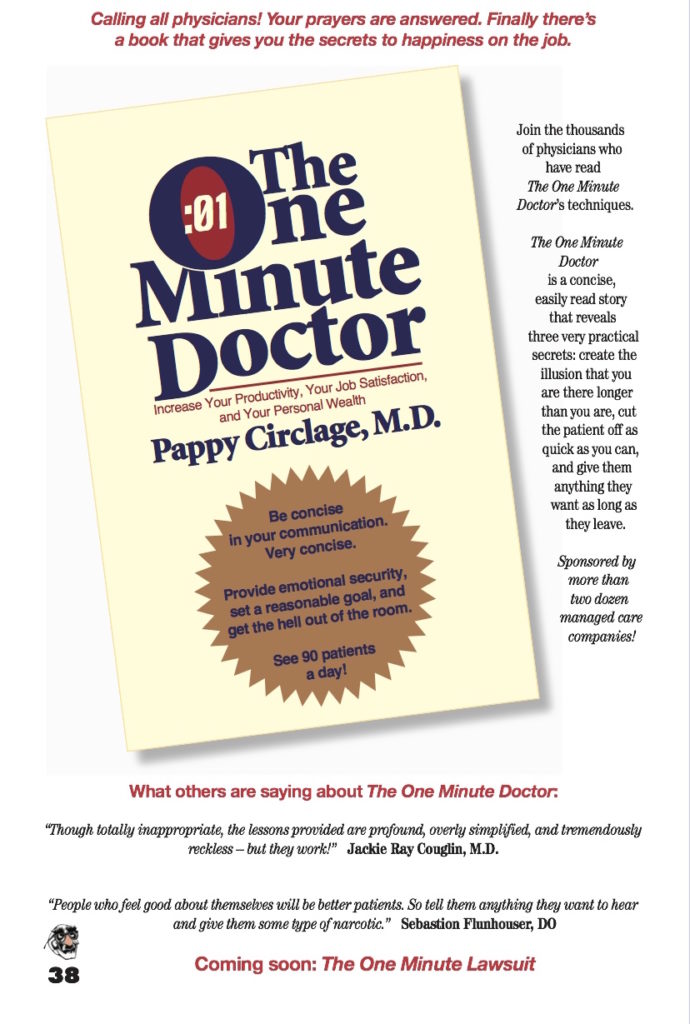
(Editor’s Note: the image above was from the late Placebo Journal, which Dr. Lassey was a major part of for almost a decade)









Go into the “wrong payer mix” area where they are too used to sucking off the government teat and you will go bankrupt with DPC. Large population of Medicare aged people? Weeellll, If you’re not accepting Medicare, you’ll not be able to fill out any of their so called paperwork for test strips, canes or wheelchairs.
Bottom line in DPC is choose your area wisely or you’ll go bankrupt like many a private practice did before you. If you start DPC relatively early before all the “good spots” are taken, then you’ll have it made. Especially if you don’t have to do call work or see people in the hospital anymore.
I have had three healthcare professionals in the past ten years that did not make me feel rushed, took time to listen, and were prepared and knew my medical history before they came into the room. One was a nurse practitioner, who not only changed my negative views on N.P.s, but has now been my primary healthcare provider for many years. One was a podiatrist who determined before he came into the room that he wasn’t the doctor I needed because he checked the results of the tests that other doctors had ordered. He still took time to talk to me and answer questions about those results since nobody had even informed me that the results were in yet. Then, by simply touching my foot, he realized that one of the test results was wrong and called the lab and discovered that, while the data was correct, someone had ticked the wrong boxes for the results. The third was a rheumatologist who was short on time with me because he squeezed me in months before he actually had an opening in his schedule. Even so, the situation was explained to me and, rather than shortchanging me or his other patients, I was asked to expect to be their for an extended time while he popped in and out of the room between other patients. Again he was prepared before he even came in and never seemed as if he was rushed or having trouble keeping things straight. He also correctly diagnosed the problem and got me effective treatment for it. One of them works for a large low income health provider and the other two work for the same large hospital. So there are doctors providing good healthcare within and despite the system. Alas, they are mostly few and far between.
– A patient’s perspective with a little more knowledge of the U.S. healthcare system than is average.