Losing Altitude by Pat Conrad MD
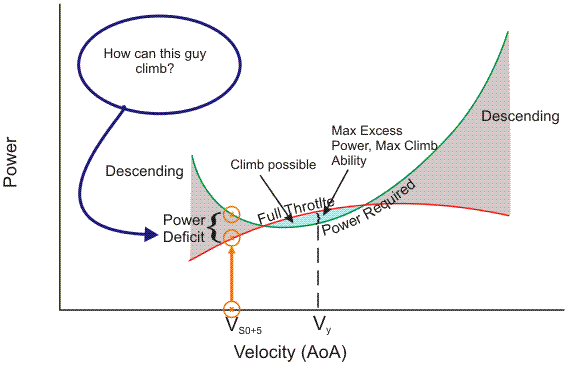
The popular phrase “behind the power curve” comes from aviation. It typically describes the situation where there is so much drag – parasitic and induced – that the available power for the aircraft cannot arrest the increasing loss of altitude. Nose high, low and slow, with the throttles firewalled and if you are too low to drop the nose and pick up speed, then…crunch.
A couple of companion articles from the Medical Economics site give a sad parallel. There are so many things dragging primary care down that medical schools lament being unable to point students in that direction. Large debt loads, a lousy pay:effort ratio, degrading work environments, and negative faculty and mentor attitudes are all major contributors. Medical schools have convinced themselves that minorities are more likely to go into primary care, and so try to direct their recruiting. Academicians worry that “Physicians in the outpatient arena are often stressed out, and that might produce negative learning, with students finishing a rotation and saying, ‘I know I don’t want to be someone who’s at the office until nine every night completing electronic health records.’” Their response: “We look for places where team-based care is happening, with teams that work together and everyone is practicing at the top of their scope.” Predictable responses promising predictable results… A fourth-year med student and chair of the American College of Physicians Council of Student Members is consulted, and assures us that the “lower earnings and higher stress levels than many of his classmates…will be more than balanced [by] the benefits of establishing long-term relationships with patients, and contributing to whatever community he settles in.” And he’ll be able to look forward to long weekends with fellow ACP members, debating on how to further advocate for new policies to encourage more primary care participation. While none of this hand wringing at the medical school level is new – it was in full force a quarter century ago when I was a student – it is amazing to me that the worries, approaches, verbiage, and naiveté have not changed one bit.
So what has changed? While everybody and their brother has loaded down PriCare with every bit of useless weight and drag they could, some other moneymakers keep inducing a little drag of their own. Medical Economics is wondering, “Will retail take over primary care?” They cite the CVS MinuteClinic and a newer Dr. Walk-In Medical Care that is beginning to staff physicians in pharmacies: “The physician offers episodic and semi-urgent care, but does not invest in a PCP-patient, long-term relationship.” Ha ha, and why the hell would he, with all the EMR-driven team building that entails? The rise of the pharmacy clinics has been fueled by lower cost, convenience, and sticking to minor, quick-fix problems while sending anything difficult back to the PCP or the ER. And after you get a quick blood pressure check, you can grab some snacks, a six-pack, some batteries for the remote, a get-well card, and be back home before its time for the next contestant to sing.
But surely these kiosk clinics can’t supplant PCP’s, right? “Will PCPs be able to compete and bring the business back? Or will primary care further splinter and become just ‘the easy stuff’ with still fewer graduates choosing primary care as a career? As long as most PCPs cannot or will not offer relationship-based care to a limited number of patients per day, these clinics will expand to fill the gap.”
Relationship-based care for a limited number of patients per day is an expletive-deleted, howling joke in the days of quality measurements, mandatory EMR’s, and looming widespread pay-for-performance. It is unconscionable for medical school faculties to encourage students to pursue primary care in this environment. Office primary care is badly underpowered and overloaded, rolling into a short final, trying to pull its nose up to keep altitude with retail alternatives. The only way to avoid drilling into the dirt is to lighten the load, and the only way for existing physicians to do that is DPC. There is no future behind the power curve.









It’s called hanging on 4.5 years to retirement. No student should consider primary care period.
Why go into debt? Get paid crap in the end to pay back their student loans?
DPC? Nice work if you can get it. So come out of training in debt, make the wrong decision
where to practice DPC, and can go bankrupt after making a go of it and regret forever one’s vocation choice. I respectfully differ here from Doug as he mentions it all depends upon marketing DPC. Well pick the wrong geographic area where the majority of patients are sucking at the government teat, they’ll continue to do that so they can continue to afford cigarettes, beer, convenience snacks let alone pay “you” a monthly fee. We had something like that in the past. It was called private practice and in the bygone era it was close to DPC except fee-for-service.
The Doc could “adjust” their fee to the patients means if they desired. (Now that’s generally
against the law!)
Get too many “high-maintenance people and lose your shirt over it. (True a DPC doc has the
option to pick and choose but nobody is perfect. Perhaps if the “drone” doesn’t pay their monthly fee it’s easier to kick them out)
Why go through all that trouble as long as a resident kisses enough a– to get a decent fellowship and get 5 lucrative job offers before they’re out of training? Yeah they gotta work their tails off but they’re better off in the end.
In the 5 years that I did primary care internal medicine, I estimate the overall climate worsened by about 15-20% per year until the day I simply had had enough and called it quits and became a hospitalist. Best decision I ever made. I don’t know how you guys still do it. More power to you but I’ll run out my time as a bootlegger.