A Tragic Comedy of Errors
And here we go again….yet another article with opinions by so-called “health policy experts” recommending the unsupervised (“independent”) practice of nurse practitioners (NPs), without doing the requisite homework before offering their uninformed perspective. So much for responsible reporting.
The entire issue of NPs practicing unsupervised is not a new one. What is different is the political agenda on which it is based. With no questions asked by any reporter or health policy expert. Why?
- The American Association of Nurse Practitioners (AANP) has mandated that 100% of all practicing NPs obtain the doctorate of nursing practice(DNP) degree within a specified period of time. Surely one must ask how valuable is a degree, an online one no less, which can be obtained by 100% of practicing NPs? In addition, all master’s programs for budding
NPs are due to be phased out and changed to or replaced by doctorates of nursing practice(DNP) curriculums. Why do these mandates not raise a red flag? - Per the AANP, the number of practicing NPs in the U.S. has increased exponentially since 2007. From 120,000 to 270,000 as of January 2019. There were approximately 250,000 in March of 2018. An explosion of 20,000 NPs within one year?
Proliferation this rapid does not occur without the rapid expansion of nurse practitioner programs. Now, if programs are developed that quickly, how is it possible that the quality does not suffer?
The fact is the quality does indeed suffer. It is no secret that the AANP is well aware of the unregulated expansion of substandard online (and some brick and mortar) degree mills, yet they continue to push their agenda that ALL
Physicians for Patient Protection (PPP) is the one organization that is speaking loudly about this issue, regardless of the vitriol directed against us. We did not form out of thin air, we formed out of necessity. None of us needed another job nor did we want it. It came to us by happenstance. Because a few concerned physicians began asking questions about the number of patients they were receiving who had been grossly mismanaged and somehow ended up on their doorstep. Because the mistakes just did not make sense for patients being managed by highly trained physicians. Errors for which a medical student would be reamed. Who else would be expected to address these cases besides attorneys? We did what physicians should do if they honor their oath. We decided to find out what was occurring and why–to protect our patients. We were just as ignorant to the issue of degree mills and “independent” practice as legislators, reporters, health policy experts, physician colleagues and other health care professionals. But we soon found out because we did our homework. No reporter has asked about that either. The stories are dismissed as anecdotal. But to the family that is affected, that anecdote is their father, their sister, their grandparent….their child.
NP runs a hormone clinic in Texas
which prescribes thyroid hormone and high doses of testosterone. A primary care physician(PCP) in the community becomes aware of the clinic when one of her patients develops polycythemia due to excessive testosterone supplementation. Supervisingphysician for NP notified and stops supervising. Complaint submitted tonursing board (BON) who does nothing. NP hires two more supervising physicians miles away and continues to practice.Same PCP informs new supervising physicians and is ignored. PCP reports them to the Texas Medical Board (TMB). Another patient of the hormone clinic subsequently dies from a heart attack. Autopsy concludes contributing cause as excessive testosterone. No action by BON. PCP notifies DEA who investigates and determines NP is not qualified or trained to prescribe some of the hormones dispensed from his clinic. BON finally suspends NP license. Another NP in the same clinic assumes care and the practice continues.Clinic is subsequently shut down after a child develops thyrotoxicosis after being misdiagnosed and given unnecessary thyroid hormone treatment. Second NP surrenders license. All three physicians brought beforeTexas Medical Board. Child recovers.**Failure to consult the supervising physician.
**Failure to stay within
scope of practice(SOP). https://kfdm.com/news/local/southeast-texas-nurse-practitioner-surrenders-license-optimum-clinic-evicted
Seven-day old neonate with vesicular rash seen by NP in urgent care. Diagnosed with contact dermatitis and Mom sent home with instructions to treat with calamine lotion. Mom suspicious of diagnosis and goes to ED where
patient is seen by a physician. Septic workup performed,patient placed on IV acyclovir for Herpes simplex infection and admitted.Patient did not have sepsis or meningitis and did well.**Failure to recognize
potentially life-threatening infectiousdisease inneonate .**Failure to follow
national medical standard for treatment of neonate with HSV.
Elderly patient with long-term psychiatric illness that had been stable for years is admitted tonursing home. Primary care NP for nursing home abruptly discontinues psychiatric medications based on advice by an inexperienced pharmacologist with no review of records, no discussion with family and without consulting the psychiatrist on call. Resultant decompensation psychosis occurs. The patient continues to worsen. NP subsequently recognizes the error and restarts the patient’s medication at the previous doses prior to discontinuation which not only did nothing for the acutepsychosis also led to a severe movement disorder. Ultimately patient is admitted to a psychiatric unit for stabilization and management by a psychiatrist. Unfortunately, the patient has not reached the clinical and psychiatric stability they had prior to the inappropriate discontinuation of their psychiatric medication.**Failure to recognize the risks associated with abrupt cessation of psychiatric medications. , but**Failure to consult psychiatrist on call.
individual Middle agedseen in the ER by an NP for severe eye pain. No eye exam, visual acuity or eye pressure documented. Pt sent home withdiagnosis of corneal abrasion and instructions to follow up with ophthalmology. Seen by oph tho days later and diagnosed with acuteangle closure glaucoma. Multiple interventions performed immediately without success andpatient was emergently transferred to glaucoma specialist at a tertiary center.Patient treated with IV mannitol and admitted.Patient subsequently had surgery; however, they were unable to save the patient’s vision andpatient is permanently blind in one eye.**Failure to recognize the signs and symptoms of acute
angle closure glaucoma.**Failure to perform an appropriate eye exam.
**Failure to consult supervising ER
physician .
Older patient seen by an NP in a rural, critical access hospital that uses on-call physicians. NP notifies the on-call physician at the insistence of a staff member and advises physician that patient “is not that sick” but needs to be admitted. Physician requests vital signs which are grossly abnormal and informs NP they are on their way in to see patient. Physician then calls ER nurse and instructs nurse to provide certain emergent interventions until physician’s arrival. Ultimately, patient is admitted to ICU and treated for septic shock. Patient survives. Physician lodges complaint which results in enactment of strict policies on when MD/DO should be notified by NPs of patients in said ER.
**Failure to recognize the signs and symptoms of sepsis, including abnormal vital signs.**Failure to institute rapid intervention for septic shock.
**Failure to notify on call ER physician expeditiously regarding critically ill patient.
Well appearing neonate seen by NP at an urgent care for fever. Patient subsequently discharged with instructions to mother to give Tylenol and Motrin for fever. No other instructions given. A family friend, who happens to be a physician, calls to chat with Mom and is informed of infant’s fever and that rectal temperature was high. Physician advises mother to take patient to the ER immediately. Patient is seen by an ER physician who performs a sepsis workup. Patient is discovered to have meningitis and is admitted to PICU. Infant nearly dies; however, subsequently recovers without residual sequelae. Physician friend notifies medical director of urgent care who enacts changes so that no child under the age of 2 is seen by the nurse practitioners.
**Failure to follow medical standard of care regarding neonates with fever.
Elderly patient seen by NP at an urgent care for angioedema. Patient is on an ACE inhibitor. NP advises patient that reaction is most likely due to something patient ingested and discharges patient home with a steroid pack. Patient never instructed to discontinue ACEI. Patient returns later to ED, requires emergent cricothyroidotomy and is admitted to ICU. Unfortunately, patient has anoxic brain injury and care is withdrawn. Pt subsequently dies.
**Failure to recognize ACEI angioedema, an emergent condition.
Young child brought tooutpatient Family Medicine clinic and seen by NP for increased urinary urgency and frequency. Urinalysis demonstrates glucosuria. No history of diabetes.Patient diagnosed with urinary tract infection (UTI) and sent home. NO ANTIBIOTICS GIVEN. Patientseen again a week later by another NP withcomplaint of polyuria, polydipsia, wetting the bed and 10 lb weight loss. U/A demonstrates urine very high glucose and large ketones.Point of care test (POCT) reveals glucose of >300 and a high Hbg A1C. NP correctly informs guardians patient has diabetes. Becausepatient appears stable,child is sent home with instructions to drink more water. Endocrine consult placed.Clinic callsendocrine group the next day and is instructed to sendpatient to ED. Clinic unable to get hold offamily but contact the following day.Child is taken toED and is admittedin diabetic ketoacidosis(DKA). Patient survives.
**Failure to recognize the signs and symptoms of new-onset diabetes.**Failure to consider the potential deadly signs and symptoms of DKA.
**Failure to consultsupervising physician.
Young adult patient with cancer seen by NP at clinic. Discovered to have critically low sodium. NP arranges direct admission to medical floor with no order for telemetry monitoring. IV NS ordered as only intervention. Patient was subsequently seen by physician who makes arrangements to transfer patient to ICU expeditiously. STAT chemistry reveals a drop in patient’s already critically low sodium level. While in transport to ICU, patient codes and dies.
**Failure to recognize severe hyponatremia.**Failure to transfer patient to emergency department for acute management of electrolyte disorder.
Older patient with chest pain seen by NP at a clinic. Patient advised that they may be having a heart attack and to go to ED to get “checked out”. Patient is allowed to drive to the closest hospital(which is not a PCI center). Patient seen by an ER physician and informed that they are having a major heart attack. STEMI protocol immediately activated and patient transferred to a PCI center; however, care is unfortunately delayed due to missed diagnosis at urgent care. Patient dies two days later. ER physician obtains EKG from urgent care which clearly demonstrates a STEMI.
**Failure to recognize STEMI on EKG.
**Failure to activate STEMI protocol, further delaying life-saving care to patient.
**Failure to follow national standard for treatment of STEMI.
**Failure to consult supervising and/or “collaborating” physician.
PPP receives cases like these DAILY. This is not authentic medicine. This is a travesty of medicine. And should be a crime. Every single case described above involves a physician who is also a PPP member. And the case somehow ended up in their lap. Some of our cases occur in supervised states, some do not. Although we get cases involving physician assistants, naturopaths, chiropractors, PharmDs and psychologists, the overwhelming majority of these cases involve NPs. NPs are not held to the medical standard of care, they are held to a nursing standard, although they are permitted to practice medicine without a medical license, thanks to legislators. It will be the supervising physician, or in unsupervised states, the “collaborating” physician, who will be held the most accountable, whether or not they were aware the patient existed. Why are reporters/legislators/health care policy experts not interested in this? Why do patients not matter? Where is the concern for them?
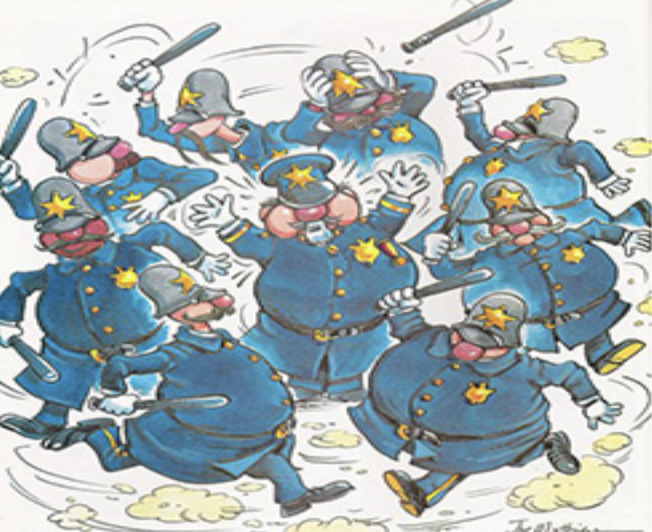
These are actual phrases and words documented in posts, charts, referrals, texts, etc. by NPs. Nonsensical terms in lieu of correct medical terminology, with which some NPs are unfamiliar. NONE are dictation or voice recognition software errors. Combined with the several mismanaged cases, it is as if we are in multiple episodes reminiscent of the Keystone Cops slapstick comedy. Except this is not funny…it’s tragic.
- “Rule out Alzheimer’s Dimension”–Alzheimer’s dementia
- “Asymmetrical ass crack”–asymmetrical gluteal cleft
- “End-stage psoriasis”–end-stage cirrhosis
- “Pre-ear infection”– “in case” of an ear infection
- “Microstones”–kidney stones so tiny that they cannot be seen
- “Loss of great-white junction”–loss of gray-white junction
- “Protein-pump inhibitor”–proton-pump inhibitor
- “Blueing of the toes”–cyanosis of the digits of the foot
- “HBP”–hypertension
- “SOE(SOB on exertion)”–dyspnea on exertion(DOE)
- “ATPPT(alert to person/place/time)”-Alert and oriented x 3
- “Lipoma follicular”–follicular lymphoma
- “Alagesic”-analgesic
- “Propothol”–propofol
- “
Nodipine “–amlodipine - “Oxygen stats”–oxygen sats or saturation
- “Growth on the neck”–enlarged lymph node
- “Audio hallucinations”–auditory hallucinations
- “Whelps”–welts
Medicine is about minimizing risk. That is not to imply that physicians do not make mistakes, of course we do. We are human. However, that fact should not sanction the unsupervised practice of NPs. One does not beget the other. Common sense dictates that those trained and licensed to practice medicine are less likely to commit malpractice/negligence/egregious errors compared to those untrained and unlicensed in it. Attorneys make errors; yet, when defendants in a criminal case wish to avoid the death penalty, how many choose a paralegal to represent them? It would be ludicrous. A defendant understands that his best chance lies with the individual possessing the most expertise in law. It is absolutely astounding to us that legislators, reporters, physicians, etc. think it is perfectly logical to allow people with no training in medicine to manage patients without any oversight whatsoever and no expectation that their practice will be held to the accepted medical standard of care. While those with the actual expertise are devalued and held to exceptionally high standards(as we should be). The commentary that no one has “heard” of any bad outcomes in unsupervised states is absurd. We’ve said it once and will say it again…absence of evidence is not evidence of absence, it simply indicates no one has looked. Maybe, just maybe, a legislator will scrutinize this most unpleasant side of “independent” practice. Or perhaps one day an investigative reporter will get off his/her a** and do what they are paid to do…investigate. Until then, patients are destined to remain in this pathetic comedy of errors.
***DISCLAIMER: THE CASES DISCUSSED ARE FACTUAL. CERTAIN DETAILS HAVE BEEN ALTERED TO PROTECT THE IDENTITY OF THE PATIENTS EXCEPT IN CASES IN WHICH THE STORY HAS ALREADY BEEN PUBLICIZED.***
(Editor’s Note: For twenty years this blog has allowed others to post their opinions here from time to time. This is a physician site so that is who it is geared towards and that is who we allow









Here’s a famous one, from Vancouver, WA.
https://www.columbian.com/news/2012/feb/04/vancouvers-former-payette-clinic-a-legacy-of-pain/
https://www.seattletimes.com/seattle-news/vancouver-pain-clinic-leaves-behind-doubts-chaos-and-deaths/
https://www.pulitzer.org/files/2012/investigative_reporting/seattle/methadone-exhibit3b.pdf
These nurse pracitioners got into the “pain fifth vital sign” in a big way. They shoveled out opiates in staggering quantities. They were notorious all over metro Portland, but no one, especially the Nursing Board, did not want to hear complaints and reports from physicians. Doctors are just those evil, corporate, you know.
They were dispensing oxycodone up to a thousand mg daily for benign pain conditions. Finally diversion resulted in a death where a family member got police involved. Then the Nursing Board had to pay attention.
People don’t believe me when I describe the quantities of opiate dispensed. I linked a Pulitzer site, you can enlarge the picture, to see a prescription from them. Methadone 10 mg – Take 10 (that’s TEN) every six hours. There’s an enlarge function, so you can enlarge the picture to see Disp: 1200.
Physician malpractice happens. When it does there is a powerful system in place to address that. Lawsuits and medical boards, etc.
NP malpractice is supervised by the Nursing board (which is not adequate to address medical malpractice issues). See above example and link.
It is up to NPs to clean house and raise standards, stop degree mill diplomas and provide rigorous research.
It is not the job of docs to find a way to work with NPs (docs suggestions of working with NPs as true extenders – for patient education, taking history, streamlining care by helping with overwhelming paperwork requirements, aiding with close follow-ups etc. – are often rejected out of hand.) Additionally, the AANP markets NPs as physician replacements capable of “independent practice.“ This is not an environment conducive to “working together.”
It is, however, up to docs to inform the public of patient endangerment (as required by oath) when the corporate medical system substitutes less trained persons to do the SAME job.
This article has very well pointed out the dangers (patient death and morbidly) when a non-physician is trying to do a physician’s job.
The public needs to know.
I think “our experience” – the experience of many of us who have worked with NPs or had an NP diagnosing or treating us or our family has been often scary and/or misinformed, as described by the authors of this article. Very unfortunate but sadly true. Otherwise we would not find the need to sound the alarm. As mentioned previously some of us are retired and have no career financial stake in this issue.
NPs who have generous nursing experience before coming to the NP field, who have NOT gone to a online degree mill, who have a healthy respect for all they haven’t learned and been exposed to in their shorter training, and who are supervised in real time by a physician are not the main subject here.
However, these* NPs are harder and harder to find.
The public should know this.
The public should know if they are seeing an NP who is not supervised or who is minimally (< 5 percent chart review after the fact, etc) supervised. The public should be aware of the training gap. The public should know if the facility or clinic does not have a physician on the premises. The public should know if an ER or ICU has no physician overnight or after hours. The public should have a choice. The public should not be pressured by the clinic or ER receptionist or scheduler to see an NP “because they are just as good.” The public should know that the studies presented by the AANP stating NP equality with physicians are not designed or statistically powered to make those statements. (Misrepresented “bad” science). The public should know if the NP they are seeing makes a malpractice mistake (just like doctors sometimes do) that NP may be held to a nursing standard of care in court (if the patient is able to find a lawyer willing to take the case (since that NP may have a lower malpractice coverage and no deep pockets behind him/her).
See here for education gap…
https://www.tafp.org/Media/Default/Downloads/advocacy/scope-education.pdf
The public should be educated to the issues. And have a choice!
Unfortunately the AANP is providing misinformation to the public…
And choice is becoming more and more limited.
Long live the PPP! We need a tagline. Something that encapsulates the underlying issue. Medical education, training and expertise matter, something like that, overstating the obvious. After finishing med school, studying full time for 4 years (not online, but in classrooms and hospital wards), I started my internship. I was confident in my knowledge base. As the months of internship grinded onwards (emphasis on the never ending grind, for those who never spent more than 100 hours per week in the big house “hospital” and being pimped unmercifully in sit down rounds by gifted clinicians ) began to realize how shallow my knowledge base truly was. Humbling. Spent the following residency years trying to become competent. If I had one bit of knowledge to pass on to NP’s independently practicing it would simply be “you don’t know what you don’t know”. Consult someone who knows. It may save a life.
This makes a lot of sense.
Until the public recognizes what is happening and speaks up to their legislators and insurance companies, this insanity will continue. The only ones benefiting from the substitution of nonphysician providers for trained physicians are the corporate practices of medicine (big hospital groups, companies staffing Urgent care centers and ERs, CVS clinics, insurance companies, etc.) They can pay nonphysician providers less while keeping the majority of payments. Yet patients must pay the same copay as if they’d seen a real physician – No patient discount for seeing a lesser trained individual. And when disasters occur, the nurse practitioners are not required to have the same amount of malpractice coverage so don’t expect them to be held financially liable. It will take an astronomical judgment against one of their corporate employers before the madness stops. Otherwise, they just view it as the cost of doing business.
Brilliant legislative strategy of starting in smaller, more rural states and selling “access to care” before moving on to badger the others for being odd to have objections. Saw this coming.
Matthew, VERY astute. This is how it works, exactly. Remember the institution of “seat belt laws” ?? Police were NEVER going to ticket you for not wearing a belt, BUT if they nabbed you for something else, they would throw it in.
And NOW? You get stopped solely for not wearing a seatbelt. No one remembers the prior promise.
In response to SP, there are few reporters anymore. The journalism platforms just don’t have the time to dedicate to this problem.
My Mom fell while on hospice and broke seven bones, over ten years ago. Admitted in the evening for pain control, the NP had her 75mcg/hr fentanyl patch removed and gave morphine 5 mg q 4 hours prn. Worse, I was there for her H and P, which just consisted of her stopping in to say one or two things and then ask “Is there anything I need to know about your Mom that I don’t already?”
PPP is a cult hate group. They do not look for solutions for problems within their own profession, and rather, deflect, deflect. There ar ex thousands more cases of ohysicians mismanaging patients. The group resorts to attacking NP business, sending threatening emails, and making false complaints to nursing boards. No, not a great source of information.
I will allow this one comment so they (PPP) can respond. There will be no more attacks after that.
A “cult hate group…” ???
Just so we can place this is context, it is impossible to get a group of 10,000 physicians from across the nation, representing multiple specialties, to form for the sole purpose of “attacking” NPs. We practice medicine and have families, we are a bit busy for that kind of nonsense. We formed by happenstance because a small group of physicians noticed a trend of patients being grossly mismanaged. What did not make sense is that the mistakes would not have been made by medical students. Thus, if physicians were making these mistakes, they needed to be removed from circulation. But the trail did not lead to physicians. To our surprise it led directly to nurse practitioners. Practicing as physicians, unsupervised. And we did what every physician with a conscience and who honors their oath would do, we set out to find out why this was happening so we could protect our patients. We discovered why. The unchecked proliferation of nurse practitioner online degree mills, spitting out NPs by the dozens like an assembly line. Who then subsequently became certified, without any nursing experience, free to practice on patients like guinea pigs. Turns out the American Association of Nurse Practitioners(AANP), and plenty of individual NPs, knew all along about these unqualified NPs and these degree mills, and did absolutely nothing. They said nothing to the legislators who passed laws in states allowing “independent” practice. Instead, they chose to push for “independent” practice of ALL NPs, including those that should not even practice as nurses, let alone NPs. All this deceit to fill a “physician gap” that should be filled by physicians since we are the only ones trained and licensed to practice medicine. With no concern as to who will fill the nursing gap that is much greater. It should be no surprise to anyone that errors such as those in the article would occur. What does one expect if one is allowed to practice as a physician without actually being one?
If you are witnessing the huge number of physicians making egregious mistakes and not reporting them, you are complicit and just as guilty. As clearly stated in the article, we contact physicians/medical directors who are inappropriately “supervising” and provide them an opportunity to correct the issue. We will not hesitate to report anyone to the nursing or medical board who is engaging in malpractice and/or medical negligence. We are patient advocates, first and foremost.
If NPs or the AANP believe that PPP is making false reports to the nursing boards, I suggest they demand an audit of each state nursing board and allow investigators to review every…single…complaint by PPP for its validity. You are not the victim. Every patient in the cases presented in the article are the true victims. Where is your concern for them?
Cult, hate group, bullies…we are none of those things. We are the town criers and you don’t like the message. It is not that the message is not true, it is that it is. NPs are not trained or licensed to practice medicine–as such, they should remain supervised. Or the cases such as those in the article will keep happening. That’s it. That’s the message.
Some of us are retired and out of medicine entirely. Those* of us have no financial reason to spread the word of rampant poor NP care.
What could be our motivation???
Maybe to avoid (ourselves or our family) becoming a sad statistic such as presented above. Or maybe we are part of this movement because we personally (or a family member) have/has been endangered or permanently damaged by dangerous & unsupervised NP care. Hmm…
Additionally if you are such an unfortunate patient, you may be left with uncompensated damages (if NP is not carrying enough malpractice or lawyer doesn’t consider pursuing the case because NP held to “nursing standards”).
If a physician makes such egregious errors patients have many powerful and effective options…
reports to medical board, lawsuits, etc.
Nursing boards are not equipped to deal with medical malpractice. As evidenced by cases where NP error left pts dead, and NP still allowed to practice – sometimes in a different state.
See below for such a case: (& Look up NP… to find new practice location)…
https://www.medicalmalpracticelawyers.com/emergency-room-malpractice-2/6-1m-oklahoma-medical-malpractice-verdict-for-death-of-19-year-old-in-er/
Patients should be informed of the education gaps and be able to choose a physician for all diagnosis and treatment if they prefer.
(Currently Some Clinics, ERs, Urgent cares, and ICUs do not have physicians on the premises! – as in case above! This leads to NO CHOICE for patients.)
Buyer beware! Patients be educated!!
Maybe we are in this movement because we are personally scared ? to death? of finding ourselves in a situation with no choice to see a physician and ending up maimed or killed by the actions of an unsupervised and overconfident NP who was practicing to the “top of his/her license”.
Hmm…
What you said. I have retired and am worried to death.
There are many APRN’s and PA’s who have worked for years gaining the trust of physicians and patients alike. We have stood by while expecting that all APRN’s and PA’s were made equal. This is far from the truth. APRN’s receive 3% of the training hours of physicians, many of them now on line. If they treat the same patients after graduation, who is more likely to make an error of judgement based on lack of training and experience. It’s common sense. Legislators and Administrators are directly responsible for the litany of errors that can and have harmed patients. I speak from a space of humility as I once was a PA who graduated from an Ivy League University, who recognized that I could do so much more for my patients if only I had the clinical acumen that I would have received in Medical School and Residency.
I am a physician and believe that NP/PAs have a role and fill a need. I work in a busy ER and these individuals are qualified to take care of simple ESI 4/5 cases and are suitable and appropriate to work with in a SUPERVISED capacity. I have seen so many insane cases like those listed on this post. Crazy near misses or misses that could have been recognized by anyone from a 3/4 year med student to an intern. I work with residents and the first year doctors require a lot of supervision to help mold them into the great doctors that eventually become, through experience, structured education, and self study but this is precisely the reason they do a rigorous 3+ year residency. I should add that they become great doctors because of the rigorous study that they undertook during medical school and demonstrated competency by passing the step 1,2,3 examinations.
NPs require no such education or rigorous testing. They simply don’t. They don’t practice medicine and they’ll be the first to tell you that. They practice “advanced” nursing. They aren’t trained to see what they don’t know. That is what makes them dangerous. When confronted with this, they get defensive and point to mistakes that they have caught in regard to medication errors by first year doctors who are being SUPERVISED.
They tried to take step 3 at one of the top NP schools and had greater than a 50% failure rate. Point being, they shouldn’t be unsupervised. They need help and supervision. They should not be “practicing at the top” of their license, whatever that means, because the top of their license is a voodoo term open to interpretation, based on bedside. Rising experience, and is in no way equivocal to medical school or a rigorous residency.
You wouldn’t want a paralegal representing you in court, which is why paralegals aren’t lawyers. The same way a airline flight attending isn’t a pilot. Just because she has been on 1000+ flights, doesn’t make her qualified to fly the plane. Same holds true with the NP practicing medicine.
As for-profit medicine continues to devalue physicians in the name of profit, we will continue to see this shift. NP’s and PA’s are cheaper for big hospital systems and therefore make them more money. As are most things, this is all about the almighty dollar.
sadly true
A reason to support pay parity for NPs.
If a hospital/healthcare system is required to pay similar rates for MD/DO to NP for the same work, then perhaps they will favor hiring MDs for those positions. You may eventually just see the best people hired for that specific role. If you’re right, then it will just be MDs, but maybe not…
I live in a small town in which I lived previously 20+ years ago. When living here then the medical service here was very good. Now it has been privatized by a large corporation and it is sad how the medical practice has deteriorated. They have driven out many doctors and replaced them with NPs who are much cheaper. Luckily the two that I have been forced to see are very good and well supervised, and luckily I am a very well educated patient who knows if something doesn’t sound right. I wholeheartedly agree this about most everything else – the almighty dollar.
So what you’re saying is that the NP care you received has been very good. Your assumption is that this because they are “well supervised” and/or because they are individually exceptional. What evidence do you have for these assumptions?
I have worked in full practice and restricted practice states. When in full practice states, as any responsible healthcare professional would, I have sought out professional consultation regularly. Some of it has been from MDs, DOs, PAs, PharmDs, PayDa, LCSWs, and of course NPs. . I choose who I consult with based on my assessment of the clinical skills. I’ve also had some really poor supervision forced upon me because my employer believed NPs should be supervised by a physician. As someone who is experienced, has taught medical students, residents, NP, and other health professionals I would STILL be forced to hire supervision in a restricted practice state. They could be shit. They could be right out of residency. They could be a sexist old dinosaur (as has been the case more than once). That’s a problem.
So you’re throwing the gender card to cover up for your fraudulent premise. You are not a physician, and any claim to equivalency is pure dishonesty.
“Playing the gender card”? Okay….I don’t really need your validation of my experiences. I encourage some self reflection on your choice of words. It doesn’t sound like this will be a fruitful conversation that will lead to better understanding of ourselves and one another.
But to be clear, you think the law should be that NPs should always be supervised by a physician, indefinitely, regardless if a NP has significantly more experience?
We don’t “play doctor” (as some reference here) and to say we claim equivalency would not be accurate either. What we claim and aim is to provide top quality care within our scope and training. What we ask for is self governance, just like our other colleagues in healthcare.
For the record, I have wonderful professional and personal relationships with physicians. I want great things for them and your profession. I would never expect commentary like that found here from any of them.
This will be the last comment from me. I was drawn to your article by the AANP response, but this is not a useful medium for meaningful engagement.
“ They could be a sexist old dinosaur (as has been the case more than once).” Your words.
Yes, I have have reflected on my choice of words, and they are precise. And it’s lucky you don’t need my validation because you damn sure don’t feel the need to earn it. You are hiding behind touchy-feely drivel like “meaningful engagement” as a failed attempt to act the aggrieved party, and divert from what you seek, which is a false equivalency. You state simultaneously the desires to proved care “within our scope” and for “self-governance.” That is an obvious contradiction, and proof that you are dissembling regarding your true motives. You and yours seek to stimulate need for yourselves by devaluing physicians, and it’s high time you were plainly told so.
As a layperson, It doesn’t make sense to me that nurse practitioners would be legally allowed to practice independently in all settings. The logical inference of such a proposition is that the extra medical training and education needed to acquire medical board certification and to head a medical team really is not necessary from the public’s point of view. In our gut, we all know this is nonsense.
My husband was one of the cases reported to PPP. He lived because of the intervention of a seasoned cardiac surgeon and a pulmonologist.
Thank you for the comprehensive report. It is astounding that reporters are not interested in this story. What do you think is the reason?
IMO, because of the animosity and resentment towards physicians is greater than the fact that we are patient advocates. Physicians are perceived as bullies while nurse practitioners are viewed as the victims, when in reality it is the patients who are the victims. It is irresponsible and unethical for any health care professional who witnesses the type of mismanagement described in the article to ignore it. Yet, it happens. It is what is referred to as the normalization of deviance, described as: “The gradual process through which unacceptable practice or standards become acceptable. As the deviant behavior is repeated without catastrophic results, it becomes the social norm for the organization.” The difference is that the catastrophic events are occurring; however, they are disregarded for a multitude of reasons.
These patients are invisible and thus, garner no interest from reporters, legislators or the public. The vitriol against physicians is much more exciting. Where there is no oversight regarding the safety and care of patients, these type of incidences will continue…until it happens to a very public figure.
Great points all. And I still suspect lazy “journalists” would like to play into defunct stereotypes of mean ol’ men doctors picking on selfless female nurses who are just trying to compassionately fill in the gaps. That pairs great with income envy when one is serving egalitarianism.
I appreciate your focus on patient safety. But,are you implying all nurse practitioners are dangerous? What has been your experience working with advanced practice providers?
And as with medical organizations, Big NP has recognized the cash cow value of mandated online CME, a force multiplier for political clout despite the lack of professional expertise.
The money, and accrual of power are excellent vehicles to exploit the poor self-esteem, and stoke the angry egalitarianism of NP’s who want to play doctor. You are phonies who have to double-down, much to the delight of payers looking for cheaper workers.
Seriously what’s wrong with you haters. Get your facts right. There is no mandate for NPs to get a doctorate. Try to work collaboratively. I can tell many physician malpractice stories but how is that working together? It’s on that individual. The fact is that the healthcare system needs all of us. I am confused about your goals. What do you want to see happen? How do you feel NPs are best utilized? How do you feel you can be more constructive?
We have a serious nursing shortage. Where is Big NP on THAT?
The public would be much better served by a lot more good RN’s rather than NP millS cranking them out.
Where would I like to see utilized, constructively? Being supervised by physicians.