Tele-intensivists
Our local hospital sent out a press release. It turns out our hospital…
————————–
… “will soon have the benefit of the most advanced telemedicine program available in hospital intensive care units today.” The hospital “will partner with Hicuity Health®, the nation’s largest provider of tele-ICU services, to deliver monitoring by highly trained intensivist physicians and critical care specialists 24 hours a day, 7 days a week, providing an extra layer of care that enhances patient care and safety.
“This new partnership with Hicuity Health is part of our commitment to continually innovate and improve services for our patients and our community…” With the addition of around-the-clock telemonitoring by intensivist physicians to the level of quality care already provided by our ICU team and physicians in the hospital, our ICU patients will receive the highest level of medical care available today.”
“Tele-ICUs are becoming an integral part of critical care services,” noted Lou Silverman, CEO of Hicuity Health. “Our team is pleased to collaborate with the physicians and clinicians…, supporting them in providing care for our mutual patients.”
Independent studies demonstrate that this 24/7 intensivist monitoring significantly improves patient outcomes and patient safety in the intensive care unit. In a study published in the Journal of the American Medical Association (JAMA), implementation of a tele-ICU program was associated with reduced adjusted odds of mortality and reduced hospital length of stay, as well as with improvements in best practice adherence and lower rates of preventable complications. Another study published by the New England Healthcare Institute (NEHI) recommends that community hospitals with 10 or more ICU beds adopt tele-ICU care.
Hicuity Health’s team of intensivists and critical care nurses work around the clock from centralized operations centers…The program continuously monitors patient vital signs, labs, and the patient’s clinical status. Proactive data management tools identify problems before they become urgent, prompting immediate intervention when necessary. In-room audio/video is utilized during periods of evaluation or when called on by the nurse. This two-way communication enables face-to-face consultations between the bedside staff and the Hicuity Health team, ensuring that help is available when needed.”
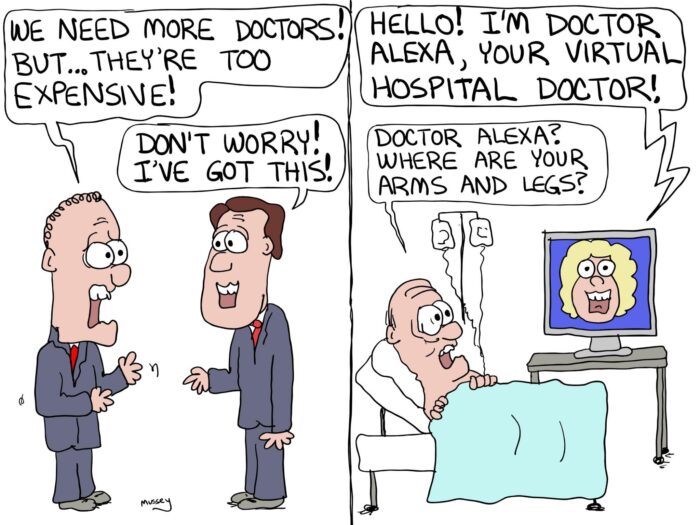
——-What do I think of this? It fundamentally violates all of the principles of my old style Internal Medicine training. I hate this virtual doctor thing. On the other hand, there is a certain reality in the ICU which has grown worse in the past two years.
In short, bad stuff happens in the ICU. The worst times to be in the ICU and unstable as a patient are night times, weekends, holidays or times of short staffing. Doctor rounding in the ICU is incredibly time consuming and complicated. To do it right, you need to round many times a day, which is something that rarely happens. Patients go from being hypotensive to fluid overloaded. They get septic or bleed. They do it when the doctor is least able to make a face-to-face encounter. In this age of Covid, doctor rounding has become increasingly distant, anyway. Over the past two years, doctors have often even rounded from outside the room, looking into the window and relying on the nurse reports. Many ICU’s rely on physician extenders and the results are often suboptimal. So, bottom line: I can see a potential improvement of care, but I’m a skeptic.









There are so many dangers to telemedicine in the ICU that I’m not sure where to start.
* If tele-ICU staff become standard practice, do you think the (corporate) hospital will maintain adequate ICU personnel?
* Doesn’t ICU usage increase during a catastrophy (hurricane, tornado, earthquake, fire, tsunami, blizzard, uprising, riot, etc.)?
* Doesn’t a catastrophy cause phone, power, internet outages?
* How is liability apportioned if tele-ICU and on-site ICU staff have a conflict?
* Has anyone asked a single patient if they think this is a good idea?
This isn’t a bad idea, it’s a damn-bad idea!
IMHO,
Jeff in Ohio
What ever happened to the now old-fashioned idea of actually examining a patient??
Yeah, I agree. They can “efff” this concept. I saw patients in the office, saw them in the hospital and took call for 32 years. Retired now but we had continuity of care. They can “efff” the concept of EHR. Worst thing that has ever happened to primary care. I was happy for my first 25 years or so but the last years s#cked. Made my life miserable and was the reason I retired at 63 (along with the fact my lovely wife died and I was sole guardian of a mentally handicapped son. Plus my financial advisor kept telling me I could retire at 60 because I saved so much.)
I dictated and signed off on my notes in office and hospital with my patients so everything was legible. EHR is simply the worst thing to come to primary care and if I had contact with med students now, I’d tell them to stay the h#ll away from this so-called specialty. It s#cks to the n’th degree and I’m glad I was able to survive to retire from it.
I hate to be so negative but if someone can get a “plum”, salaried position in primary care without call, so be it and enjoy it as long as one is compensated well.
Allen Kurt Savegnago, M.D. (retired
Canton, Illinois