The Hattiesburg Study-An Unsurprising Surprise
Mississippi Frontline – Targeting Value-based Care with Physician-led Care Teams
For those who may not know, the Hattiesburg Clinic in Mississippi is the real deal. An extraordinary clinic with a superior reputation. Congrats to them for this exceptionally well done study. The authors of this article admit that they were both surprised and disappointed in the results of the study. I will be blunt and state that I am neither surprised nor disappointed. I’ve never understood the success of Full Practice Authority(FPA) when it is and has always been evident to me that if you permit people untrained in medicine to practice it, don’t expect stellar results. I’ve also expressed that no physician is so exceptional that he or she can teach a nurse how to practice medicine so efficiently and effectively that they can practice independently. There is a reason medical school and residency are long and arduous. The Johns Hopkins model of medical education has withstood over 100 years of challenges and growth in medicine. The model works.
The Hattiesburg Clinic set up their own similar FPA-like model with “collaborating” physicians and enabled nurse practitioners(NPs) to have their own patient panels. They then did what no state legislature, regulatory or nurse licensing body has ever done in any state with FPA…they followed up–10 years later. You know, to see if what they instituted was actually working. Mad respect for this institution. There is no doubt in my mind that everything they did was in the best interest of their patients. That’s why they have the reputation they do and it is well-deserved. If every FPA state and academic center were to do the same, I predict the results would be similar. With all due respect, I think the one mistake the authors made was in believing that there was “”mounting evidence nationally that APPs could provide levels of care similar to that of physicians”.
“We allowed APPs to function with separate primary care panels, side by side with their collaborating physicians. Although necessity initially drove our decision to allow APPs to function in the primary care provider(PCP) role, we felt comfortable with this decision over the following years as there was mounting evidence nationally that APPs could provide levels of care similar to that of physicians.”
The reality is there was no mounting evidence. It didn’t exist and still doesn’t. Physicians for Patient Protection(PPP) stated this years ago and no one listened. Then PPP members, Drs. Rebekah Bernard and Niran Al-Agba, documented and debunked the studies in their book, “Patients At Risk: The Rise of the Nurse Practitioner and Physician Assistant in Healthcare”. That information was then shared in the “Patients At Risk” podcast(https://youtu.be/yGeFGndEiwA) in three episodes. Bottom line, the studies the American Association of Nurse Practitioners(AANP) use to push FPA are outdated, poorly done studies. I’ve often said, if docs and legislators took the time to review even one study, the shoddy methodology would be obvious. Unfortunately, when fiction is repeated often enough, it becomes fact. And no one is prompted to check the “facts”, they simply believe. That is how FPA has progressed successfully–that and exceptional lobbying by the AANP. My perspective of the entire FPA movement is that it doesn’t make sense–and I’m a chick with a lot of common sense. In my opinion, some things are so apparent as to not require a study. Nurses are not physicians, so how could they possibly have similar outcomes as physicians? Who would believe that s**t? Turns out, a lot of people do. And instead of asking NPs to prove what they claim with actual, respectable evidence, physicians are asked to prove a negative–that NPs are not qualified. Preposterous.
“Dr. Fitzpatrick noted that legislation to let nonphysician providers practice independently gets introduced every year in Mississippi, and this year the bill didn’t make it out of committee.
“A lot of it had to do with having real data—home-based, Mississippi-based—that was credible and published,” he said. “Our legislators did a commendable job with analyzing the information available with a focus on putting patients first and at the same being mindful about strategies to reduce the total cost of health care.” “
Here’s the gist: if one wants to practice medicine, the responsibility lies with one to prove he or she can do so effectively and competently. That didn’t happen with FPA. The one exam specifically designed for nurse practitioners with Doctors of Nursing Practice(DNP) degrees to prove their competency failed, after 5 years of being administered. Nothing has replaced it since.
I believe every state with FPA has a responsibility to do what the Hattiesburg Clinic did(which I view as a microcosm of the enactment of FPA). FOLLOW UP. Evaluate and assess if FPA is indeed working as purported. Oregon has had FPA the longest, why hasn’t an assessment of FPA been done there? Or in Arizona where FPA has been in existence since 1996? The Hattiesburg Clinic is probably one of the best examples of a MD/DO-NPP collaborative model. Yet, the results of their study was an eye-opener for them. Makes me wonder what we might see in less exemplary models…In any case, true to form, the Hattiesburg Clinic is changing its practice based on the results of their study. I would expect nothing less from such a clinic. Every institution should be as responsible and discerning. Kudos to them again.
“The practice of medicine is the gold standard by which all other disciplines of health provision are measured. The onus is on others to prove, with VALID evidence of sound quality and unquestionable standards and methodology, that their discipline measures up.”–Natalie Newman, MD









Hello All. Favor argument. I am a PA-C With 45 years experience as a PA-C.I was trained to assist a Physician,do 70 to 90% of what he does,ROUTINE Stuff, so he or she had more time for there more complicated patiemts.. IN 45 YEARS IT HAS NEVER BEEN THAT WAY.. I have been treated as a CHEAP DOCTOR.. Working 60 to 100 hour weeks, treating MI’s in the ER and transporting to higher levels of care.
Major trauma and my back up Surgeon was too drunk to safely function as he pissed off all the EMS people and I had to pause,sit the Surgeon down, in his office and have his lover keep him there. I stabilized the patients children thru grandparets and shiped them out to level 2 or 3 trauma centers.North Carolina in 1978.
Fun times had by all…..NOT. No other Physicians available.Just me and several good RNs and EMTs.
All I ever wanted was a GOOD supervisory Physician,in primary care to work with for 30 or 40 years..
Never found it. To my knowledge I never Killed anyone and when I had questions I got answers or referred to my supervisory MD/DO or to referral Physicians.Had a patient having a stroke,and could not get the local physician to come see patient.Could not get the Referral Neuro group one hour away to accept patient, so patient and his wife drove to Dallas 5 to 6 hours away.. NOT GOOD. Neuro Group was fighting with local hospital. Most upsetting and WRONG. BUT EVERYTHING IS A BUSINESS MODEL..NOT A MEDICAL MODEL.
SO KEEP ARGUING FOLKS,WE WILL WORK IT OUT ONE WAY OR ANOTHER.. Thank you all for your divrrse perspectives and opinions.Often educational,always serious and sometimes funny serious.
JESSE BELVILLE,PA-C
Thank you for sharing your remarkable experience – yes let’s all pull together and keep helping people as you have through out your remarkable career.
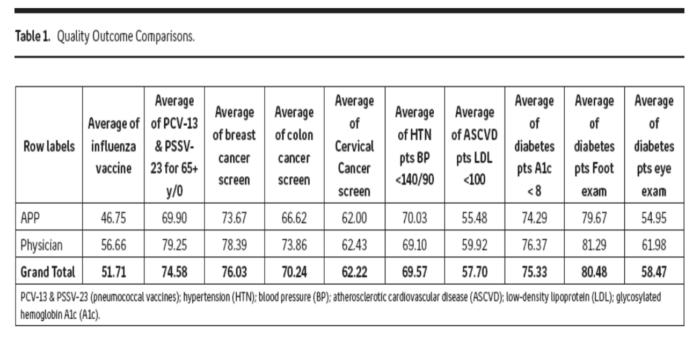
You have fallen for the fallacy of so called “quality markers” as a surrogate for quality care. I read the data as ARNPs are about as good as physicians in ticking boxes off in preventative care. Why would we expect otherwise? Any careful clerical person could make sure colonoscopies, foot checks, etc are done. A1C does imply some clinical skill. The real questions is how prepared is the ARNP when faced with a seriously ill patent, or one not already labeled with a serious disease? The results of equivalent national testing as reproduced in the opinion piece are not reassuring. I work with some of the finest ARNPs with years of nursing experience before their additional training. They handle most routine things very well. They refer to consultants and dx procedures at a lower threshold than physicians. Thus, patient welfare is rarely jeopardised, but, I am uncertain whether there is any savings to the system in their wide-spreaad deployment. It is not the pathetic income of PCPs that is important; it is the massive budgets they control or influence that spend the health dollar. Enhanced collaboration with physician co-workers will not happen under the fee for service model (both physician and ARNP are running). That will change with widespread capitation – it becomes in the interest of the providers to stem the unnecessary (but quicker, easier) referrals. When deep thought and more time becomes valued it will enhance the role of the physician and their support of the ARNP.
Sure, because capitation delivered such stellar results over the past 35 years.
Absurd.
The study looked at 300 physicians and 150 “APPs”, of which 10 were PAs. 10! This is directly from the study’s primary author.
It is absolutely telling the glee a sub-set of physicians express with studies like this.
It’s nice to see a voice of reason… Dr. Sadler (I still gave an original edition of your book!). It is time to put our differences aside and work together on a model for practice that leverages all our education and talents to the benefit of PATIENTS….you know, those people we are supposed to be helping?
I am ready and willing to come to the table. Are you?
Thank you Ed for your most reasoned response. Yes, I am very willing to help organize a discussion or be part of one on these most important matters. There will always be a few outliers who disgrace our profession, whether MD, DO, PA, MD, or others. I have a new book coming out on June 28 that deals with these and other health care matters. All the best, Fred
oops – meant to say NP as the last professional degree.
I’m a physician – how can a PA or NP disgrace MY profession?
Hi Pat, I was referring to the physicians who unfortunately disgrace our profession through incompetence, abuse of patients, improper billing, etc. The sad story of the Ob/Gyn Dean of the USC Medical School is one recent example. All physicians should not be demeaned by the bad behavior of a few. Most all of the NPs and PAs that I have worked with over the past five decades have been very good if not excellent and know their limitations. They have no desire to practice independently. Unfortunately some of the some in Nursing leadership still haven’t learned about practicing interdependently as part of a health care team. No one in the 285 accredited PA Programs is teaching independent practice. There is much more to be said about this matter but I hope this reply clears up my earlier post. We all have to take on the business people who run so much of our beloved profession – the subject for another post. Best regards, Fred
We leave that to you.
Que?
Hi everyone, This is a very important study and nicely reviewed by Dr. Newman. The “independent practice” by organized nursing has been very distressing to all of us who believe in quality care. They typically don’t say whether this is the independent practice of nursing which they have been licensed to perform for decades or whether the they want to perform the independent practice of medicine. This is further clouded by the “Doctor of Nursing Practice” Degree which is an online degree with no clinical training.
As I have commented before, let’s not lump PA’s with NP’s. PA’s are not advocating for independent practice. Historically, the PA Profession was designed in the late 1960’s to support overburdened physicians and have done a magnificent job of that. I’ll be writing more on that in another post.
Professions, as they mature tend to slip into a “guild” mentality and get caught up in “turf” battles (Optometry vs Ophthalmology) for example. We need to have leaders of the physician, NP, and PA worlds meet together and work issues out professionally. Having scope of practice issues decided by state legislatures is insane.
The David Mittman PA comment is most unhelpful. We need to avoid all forms of “hate speech” particularly in this time of unprecedented polarization. Let’s roll up our sleeves and continue to work together. Best regards to all.
“PA’s are not advocating for independent practice.” This is an absolute lie and you know it. See Maine.
please explain to this PA who advocates in a regular basis.
https://www.aapa.org/news-central/2020/03/maine-legislature-fast-tracks-pa-legislation-to-help-combat-covid-19/
Checkmate
Trojan Horse
OTP is not independent practice. It espouses all the tenets of team practice. One tenet is to relieve the physician from legal liability for the PA’s action if the physician wasn’t involved in the patient’s care. Another is to allow the practice to determine the PA’s level of autonomy based on education, training, and experience. Who best knows their PA? The people who work with them. I have been a PA for 40+ years. I enjoy a fairly high degree of autonomy. My new hire…. With 8 yrs experience isn’t so “lucky”…. But she will gain more as her clinical and procedural skills improve.
My state is one that removed all supervisory requirements at the beginning of the pandemic. That allowed us to shift and move into areas of greatest need, in conjunction with the physician and other members of the team. Did we all of a sudden get OR privileges and do craniotomies? Sure, just about the time hell froze over…. And guess what? No increase in complication rates, no increase in med board complaints, no increase in death rates (aside from those claimed by Covid), and a lot of patients who were able, who are still able, to access quality care in a timely fashion.
Again, I am happy to sit down and discuss a model for practice that is agreeable (or as close as can be) to all parties. I am acquainted with several PA leaders and you, I presume, are acquainted with several physician leaders. Dr Sadler, for whom I have the utmost respec, right up there with Eugene Stead, has kindly offered to organize. The opening discussion should be how the PA profession has evolved over 50+ years and just what “supervised” practice means. I have no issues with Physician Lead Care, as long as those physicians act as true leaders and not little tyrants.
Trojan Horse. It started the same way (small) with NPs. It’s funny, I once asked Dave Mittman PA to work with doctors to hammer the NPs and come out saying PAs don’t want independence. He said no. He wanted to stay out of the fray. Oh, it’s coming and you all know it.
For those who wonder….here is the Main PA statute. I submit, a law that requires a practice agreement is not independent practice.
https://legislature.maine.gov/statutes/32/title32sec3270-G.html
Thank you Ed for providing us with the Maine Law relating to the team practice of Physician Assistants. This is clearly not “independent practice”. It is helpful to physicians who work with PAs in several ways. Physicians are not required to review every chart. Physicians are not liable for errors made by the PA. Remember that the PA Profession was started by far sighted physicians who realized that much of what a physician did in his/her practice could be performed by a specially trained practitioner as long as the physician took full responsibility for the assistant. This was accomplished by a simple ammendment to the medical practice act in each state. Over time, as it was clear that PAs were well trained and capable practitioners, states began to develop their own practice acts for PAs. The new profession was created in response to the greatly increased demand for medical services after Medicare and Medicaid were implemented in 1966. The Physician Assistant Education Association (modeled after the AAMC) was formed in 1972 to discuss and determine matters of mutual interest and concern. As Founding Director of the Yale PA Program in 1971, I was honored to be selected as the first President of the originally named Association of PA Programs. PAEA celebrates its 50th anniversary this year, and at the ripe old age of 81, I continue to remain actively involved and am thrilled to witness the dedication of PA Educators and PA students. With nearly 300 accredited PA Programs and over 150,000 certified graduates – the Profession has served millions of patients, while working interdependently as part of health care teams. For more on PA History – go to the pahx.org website. I’ll have more to say as we go forward together. For those who need to know, I was trained in surgery at the Hospital of the University of Pennsylvania and in Primary Care Internal Medicine at the Massachusetts General Hospital. Thanks to all of you for forming this most important physician organization. Fred
Ed, I disagree. The DSA was much more protective of the physician’s license as each physician could determine what they would delegate to the PA and what they would not. It depended on their comfort level, not the PAs. The practice agreement leaves it at the discretion of the PA to determine when they need to consult with a physician, even if that PA is straight out of school or is a lousy PA. This notional supervision is useless and for all intended purposes enables the PA to practice “independently” as opposed to autonomously. This is not ok.
“…the physician will be available to the physician assistant for collaboration or consultation…”. It is that statement that places the physician at risk legally. “Collaboration” as it is used in scope creep is a misnomer. Collaboration does not have to be mandated, it is an organic event that occurs by virtue of being part of a team. When it is mandated, it is supervision. It’s just lax to no supervision. A physician stating in a chart that they were “available for consultation” doesn’t do jack for them legally. It actually heightens their risk of being sued than if they had said nothing. Absolutely nothing in any OTP bill indemnifies a physician from being sued, so stating that they are protected from lawsuits is absolute bulls**t. Attorneys are not bound by OTP. They will always seek out the physician who is presumed to be “in charge”. Only one state indemnifies physicians from being responsible for NPPs as part of the business and professions code–AZ. Physicians are indemnified from being legally responsible for CRNA’s.
“A physician or surgeon is not liable for any act or omission of a certified registered nurse anesthetist who orders or administers anesthesia under this section.”
https://www.azleg.gov/ars/32/01634-04.htm
Conveniently, the AAPA chapters pushing this s**t never asked for physicians to be indemnified. Why not? Because they don’t want to own the risk, that’s why. Telling docs they won’t be sued is nothing but lip service. Back it up with indemnification.
There is no question that OTP came about as a result of PAs being pushed out of the medical landscape by NPPs who had achieved FPA, despite the fact that have no business practicing medicine w/o a license. The AAPA decided to follow suit. Call it “collaboration” while practicing w/o supervision until the s**t hits the fan. It is no secret that physicians have been sued as a result of NPP mishaps. It is preposterous to then expect them to believe that OTP would miraculously prevent that.
I have a overbooked patient scheduled today and wanted to comment on one of your points. I don’t know which constituent organizations did not ask to indemnify physicians. As someone involved in advocacy and legislative affairs, I would like to know. One of the tenants of OTP is having the PA responsible for their own actions, Indemnifying the physician in those cases where they were not involved in the medical decision making.
Dr. Sadler, with all due respect, I really dislike when the actions of physicians who oppose FPA and OTP are dismissed as being a “turf war”. It minimizes a very serious issue and is frankly offensive. Optometrists are not trained to perform surgery. A certificate that allows them to do what an opthalmologist does, when the optho is required to have 4 years of PG training should not even be considered in the same orbit. They are not on the same turf so there can be no turf war. This is about patient safety. Why is it so hard to understand that there are some docs who have genuine concerns about patients and don’t find FPA/OTP to be harmless jokes? It’s fraud.
We don’t have to conflate PAs and NPs. The conflation began when the AAPA promoted the OTP movement which absolutely mimics FPA. That was their choice, physicians had nothing to do with that absurd decision. And they are seeking independence–there is no question about that. Whether or not the majority of PAs agree with OTP is irrelevant when the AAPA is courting legislators to pass the law in all 50 states. What are physicians supposed to do, just watch it happen when we know it’s wrong? I don’t get the passivity. If we don’t stand up to prevent these laws, then who is supposed to? Are we patient advocates are aren’t we? My loyalty is not to PAs or NPs, it is to patients.
And, again, happy to sit down with any group to develop a practice model that leverages all our talents to better serve patients.
Two things.
There were 10 PAs in the entire study.One outlier could skew the entire thing. Like possibly if the majority were just out of school?
The study has some major flaws like that.
Any good researcher would not even allow it to be published.
Sad, how much hate you all have.